Neonatal Quality Improvement 5
Session: Neonatal Quality Improvement 5
515 - Implementation of a Neonatal Pain Clinical Practice Guideline in a Level IV NICU: A Quality Improvement (QI) Initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 515.5165
Ying Ge (Inga) Wang, NYP-Weill Cornell, New York City, NY, United States; James M. kim, Weill Cornell Medicine, new york, NY, United States; Priyanka Tiwari, Weill Cornell Medicine, New York, NY, United States; Yurhee Lee, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Ilaria Mignatti, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Allison N. Weaver, Weill Cornell Medicine, New York, NY, United States; Samantha Frankenberg, Weill Cornell Medicine, Bloomfield, NJ, United States; Sara E.. Rostas, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States
Ying Ge Wang, MD (she/her/hers)
PGY3
NYP-Weill Cornell
New York City, New York, United States
Presenting Author(s)
Background: Neonates in the neonatal intensive care unit (NICU) are frequently exposed to painful stimuli, risking adverse neurodevelopmental outcomes if not adequately treated. The American Academy of Pediatrics (AAP) recommends unit-specific guidelines for assessing and managing neonatal pain. Baseline data from our unit revealed inconsistent pain assessment and management, highlighting the need for a standardized pain guideline.
Objective: We implemented a quality improvement initiative in a level IV NICU to standardize pain assessment and optimize pain management in post-operative neonates. Our SMART AIMS were to 1) improve adherence of pain assessment using Neonatal Pain, Agitation, and Sedation Scale (N-PASS) in post-operative neonates by 50% and 2) reduce the N-PASS scores in the 48 post-operative hours by 10% by the end of June 2024.
Design/Methods: We conducted a 13-month observational, time-series study (May 2023 to June 2024), starting with a baseline data from May to August 2023. A key driver diagram was created (Figure 1) and interventions included creation of a pain management guideline, updates to N-PASS flowsheet in EMR, standardization of nursing and pharmacy education. Outcome measures included post-operative N-PASS scores, and process measures included utilization of N-PASS scale and appropriate post-op acetaminophen orders. Balancing measures included cumulative morphine equivalent dosing (MED) and timing for enteral feeds. Statistical process control charts (p and X-bar/S charts) were used to display and analyze our data. Associates for Process Improvement (API) rules for special cause variation were applied.
Results: Adherence to N-PASS scoring in the first 12 post-operative hours improved from 4% to 58% (Figure 2). Overall N-PASS scores for the first 12 hours post-operatively remained at 1.4, but a trend towards a decrease in scores was observed. In addition, for those surgeries anticipated to cause severe pain, there was a center line (CL) change in N-PASS scores from 2.5 to 1.3 (Figure 3). Post-operatively, acetaminophen orders remained at 80% with no CL change. There was no change in cumulative MED and time to enteral feeds.
Conclusion(s): Implementation of a neonatal pain clinical practice guideline for post-operative patients and EMR changes resulted in significant improvements in adherence of pain assessment using N-PASS scale and a decrease in mean N-PASS scores for surgeries anticipated to cause severe pain. Future efforts will focus on further improving adherence to N-PASS scoring, reducing N-PASS scores in post-operative neonates, and implementing pain guidelines for intubated patients.
Key Driver Diagram
.png) Figure 1. Key driver diagram showing primary aims, drivers and change ideas.
Figure 1. Key driver diagram showing primary aims, drivers and change ideas.P-Chart: N-PASS Adherence 1st 12hr Post-operative Period
.png) Figure 2. Adherence to N-PASS scoring in the first 12 post-operative hours improved from 4% to 58%.
Figure 2. Adherence to N-PASS scoring in the first 12 post-operative hours improved from 4% to 58%.X-bar Chart: Mean N-PASS Score in 1st 12hr in Severely Painful Surgeries
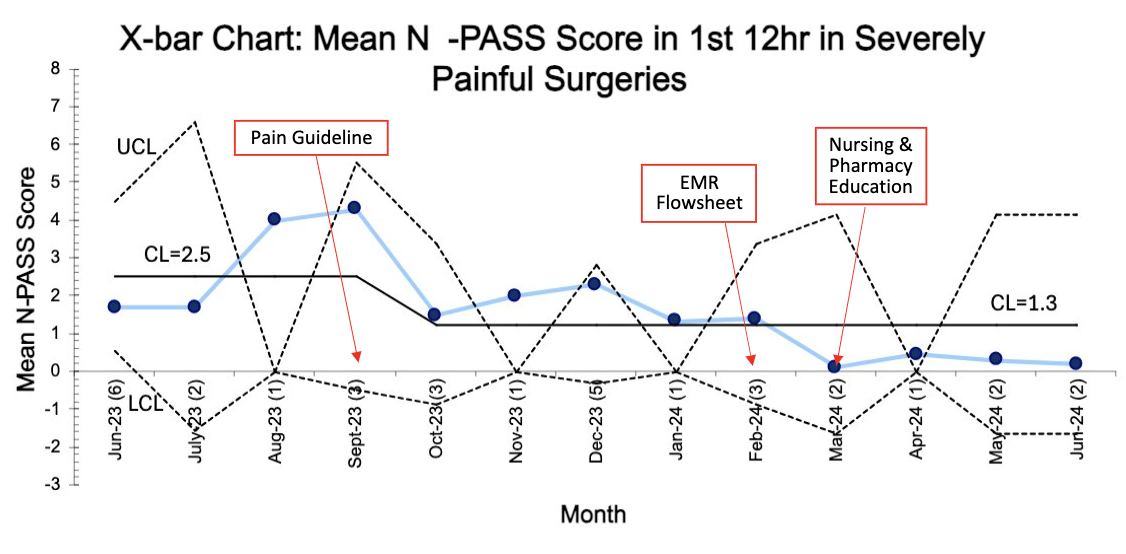 Figure 3. Mean N-PASS scores in the first 12 post-operative hours decreased from 2.5 to 1.3 in surgeries anticipated to cause severe pain.
Figure 3. Mean N-PASS scores in the first 12 post-operative hours decreased from 2.5 to 1.3 in surgeries anticipated to cause severe pain.Key Driver Diagram
.png) Figure 1. Key driver diagram showing primary aims, drivers and change ideas.
Figure 1. Key driver diagram showing primary aims, drivers and change ideas.P-Chart: N-PASS Adherence 1st 12hr Post-operative Period
.png) Figure 2. Adherence to N-PASS scoring in the first 12 post-operative hours improved from 4% to 58%.
Figure 2. Adherence to N-PASS scoring in the first 12 post-operative hours improved from 4% to 58%.X-bar Chart: Mean N-PASS Score in 1st 12hr in Severely Painful Surgeries
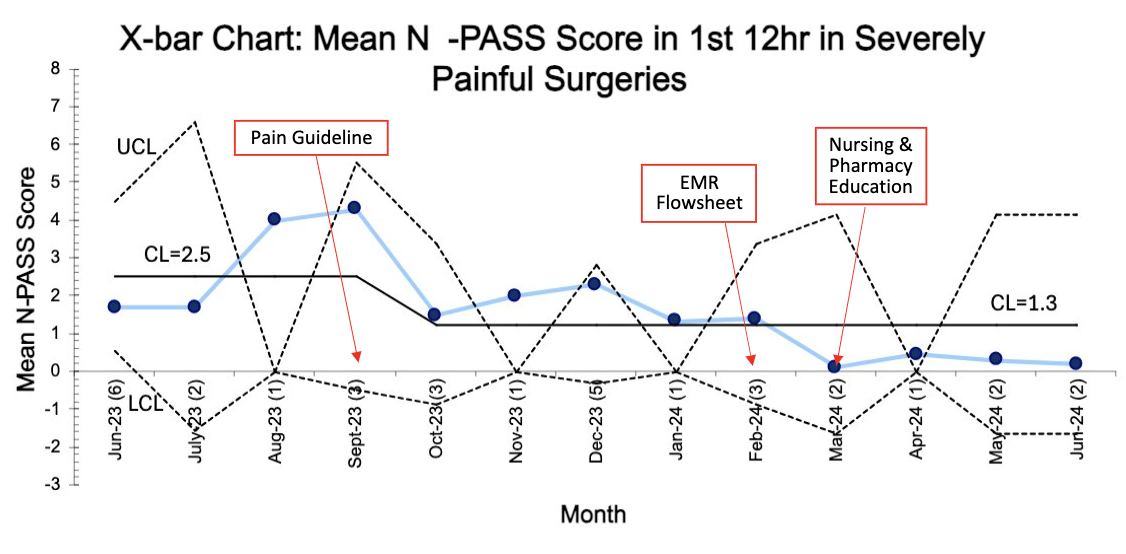 Figure 3. Mean N-PASS scores in the first 12 post-operative hours decreased from 2.5 to 1.3 in surgeries anticipated to cause severe pain.
Figure 3. Mean N-PASS scores in the first 12 post-operative hours decreased from 2.5 to 1.3 in surgeries anticipated to cause severe pain.

