Neonatal Nephrology/AKI 2
Session: Neonatal Nephrology/AKI 2
021 - Growth Outcomes After Acute Kidney Injury in Extremely Low Gestational Age Neonates
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 21.5194
Nikitha Gorti, The Children's Hospital at Montefiore, New York, NY, United States; Ako Adams Ako, The Children's Hospital at Montefiore, Bronx, NY, United States; Abner Kahan, Albert Einstein College of Medecine, Brooklyn, NY, United States; Mamta Fuloria, The Children's Hospital at Montefiore, Bronx, NY, United States; Kimberly J. Reidy, The Children's Hospital at Montefiore, Bronx, NY, United States; Mimi Kim, Albert Einstein College of Medicine, larchmont, NY, United States

Ako Adams Ako, MBBS, MPH (he/him/his)
Resident
The Children's Hospital at Montefiore
Bronx, New York, United States
Presenting Author(s)
Background: Acute kidney injury (AKI) and sub-optimal growth are common in extremely low gestational age neonates (ELGANs). AKI may impair electrolyte balance and fluid regulation, contributing to sub-optimal growth.
Objective: This study aims to determine if AKI is associated with sub-optimal growth at 36 weeks post-menstrual age (PMA) in ELGANs.
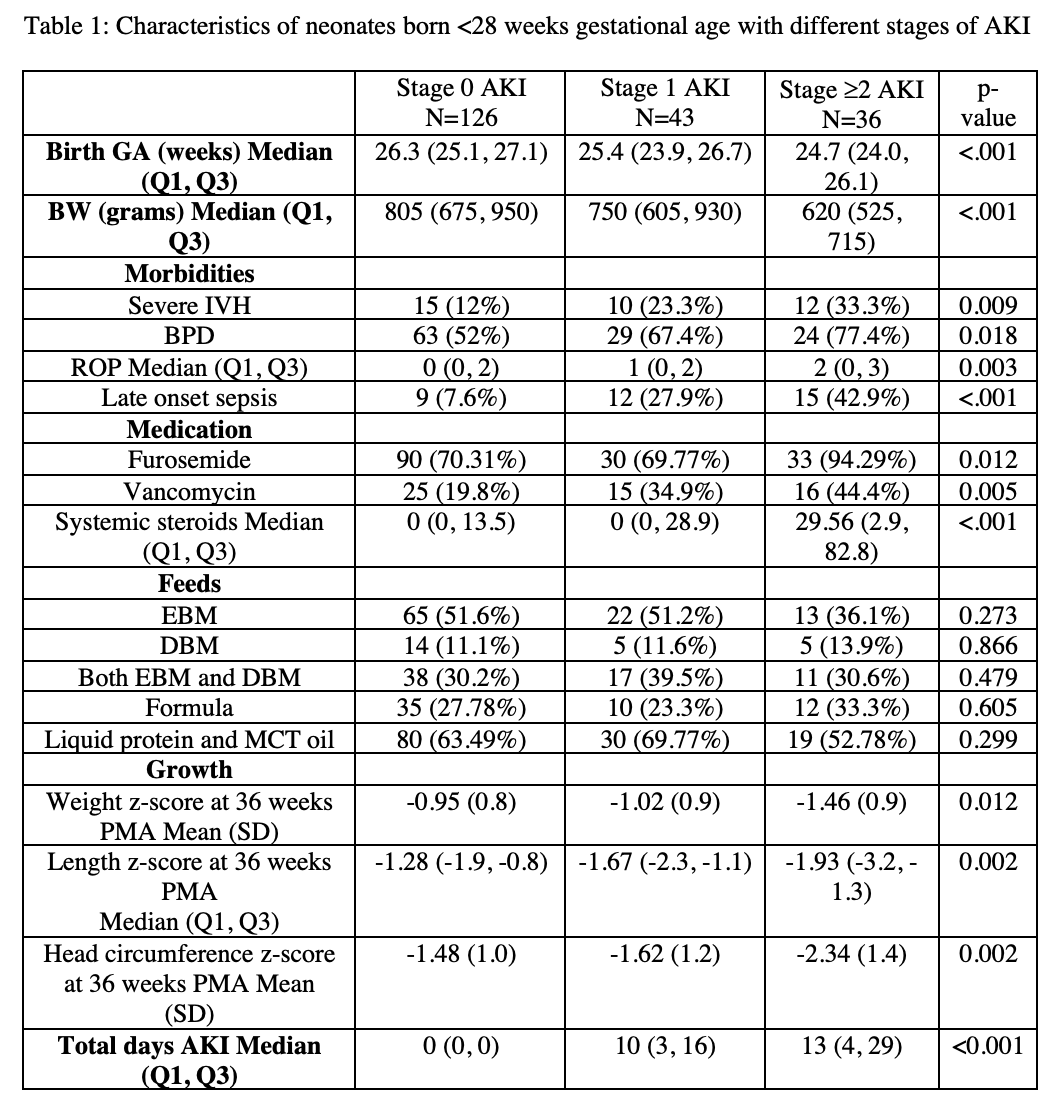
Design/Methods: A retrospective cohort study was conducted on neonates < 28 weeks’ gestation admitted within 24 hours of birth to the Weiler Division of Montefiore Medical Center from 2018-2022. We excluded neonates who expired within 24 hours of age, had congenital anomalies of the genitourinary tract, genetic disorders, or < 2 serum creatinine measurements. AKI was defined using the neonatal modified KDIGO criteria. Weight, length, and head circumference (HC) z-scores at 36 weeks’ PMA were compared between neonates with and without AKI using two-sample T-test or Wilcoxon rank sum test. ANOVA or the Kruskall Wallis test were performed for comparisons involving > 2 groups.
Results: Of 205 neonates, 79 (38%) had AKI; 18% early AKI and 20% late AKI. AKI was associated with lower birth weight (BW; p< 0.001) and gestational age (GA; p< 0.001). Neonates with AKI had higher likelihood of severe intraventricular hemorrhage (p=0.004), bronchopulmonary dysplasia (p=0.007), retinopathy of prematurity (p=0.008), and late-onset sepsis (p < 0.001). Vancomycin (p=0.002) and steroid (p < 0.001) use were associated with AKI. At 36 weeks’ PMA, neonates with AKI had lower weight (p=0.044), length (p=0.008), and HC (p=0.021) z-scores. There was no difference in the use of breast milk (p=0.431), formula (p=0.991), and nutritional supplements (liquid protein, MCT oil; p=0.832) between the groups. Similar findings were seen when comparing the late AKI cohort to the early AKI and no AKI cohorts (length p=0.003; HC p=0.005; weight p=0.076). Neonates who developed stage 2-3 AKI had median total days of AKI that was 3 days longer than the stage 1 group (p < 0.001) and had lower weight (p=0.012), length (p=0.002), and HC (p=0.002) at 36 weeks’ PMA. After adjusting for BW and GA, neonates with any AKI, late AKI, and stage 2-3 AKI still showed trends of having lower length (p=0.09, p=0.08, p=0.10), with no difference in weight and HC.
Conclusion(s): Even amongst extremely preterm infants, AKI is associated with lower BW and GA. AKI, particularly late AKI and higher stages of AKI, is associated with reduced length at 36 weeks PMA after adjusting for BW and GA. Larger prospective studies are needed to explore the relationship between AKI and infant growth parameters.
Table 1: Characteristics of neonates born <28 weeks gestational age with different stages of AKI
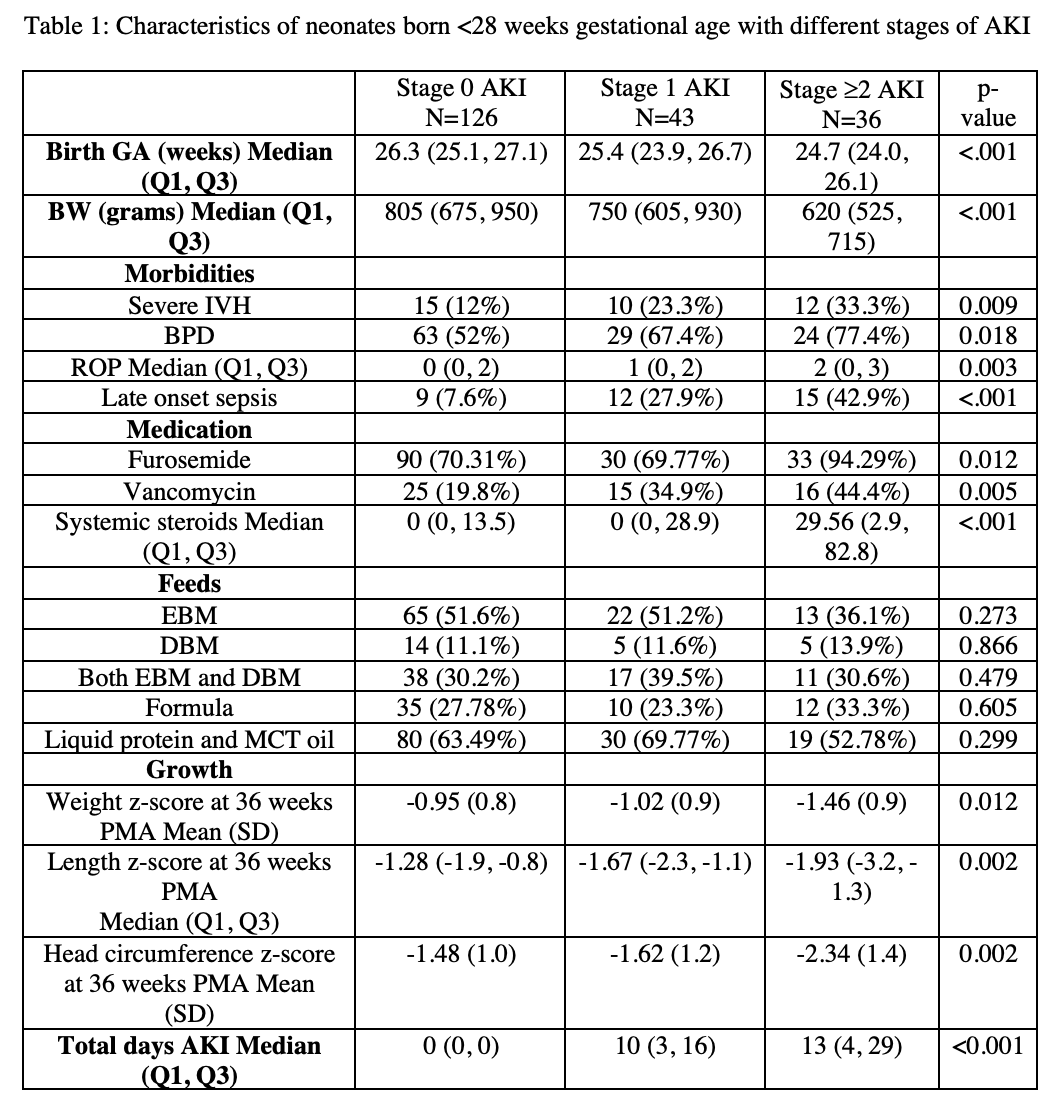
Table 1: Characteristics of neonates born <28 weeks gestational age with different stages of AKI