Hematology/Oncology 2: Pediatric Hematology
Session: Hematology/Oncology 2: Pediatric Hematology
112 - Evaluation of the relationship between hemolysis markers, transcranial dopplers and magnetic resonance imaging in pediatric sickle cell disease: A pilot study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 112.5049
Valeschia Alexander, NYP Brooklyn Methodist Hospital, Brooklyn, NY, United States; Jessica Vasquez, NYP Brooklyn Methodist Hospital, New York, NY, United States; Manoj Chhabra, NewYork-Presbyterian Komansky Children’s Hospital, Brooklyn, NY, United States; Dev M. Chhabra, Seton Hall University, Ridgewood, NJ, United States; Oksana Nulman, NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY, United States; Martin Dorciak, University of Helsinki, Brooklyn, NY, United States; Sheera Minkowitz, Brooklyn Methodist Hospital, Brooklyn, NY, United States
- VA
Valeschia Alexander, MD (she/her/hers)
Resident
NYP Brooklyn Methodist Hospital
Brooklyn, New York, United States
Presenting Author(s)
Background: An estimated 11% of children with sickle cell homozygous SS (HbSS) without screening and prevention treatment will have an ischemic stroke by age 20. The findings of the STOP trial led to the recommendation for yearly transcranial doppler imaging (TCDi) as screening for stroke risk. We present the findings of a pilot study aimed to assess the potential relationship between TCD velocities, magnetic resonance imaging (MRI) findings, hemoglobin (Hb) and bilirubin.
Objective: To evaluate the relationship between conditional TCDi velocities, MRI abnormalities, Hb and bilirubin in the pediatric sickle cell population.
Design/Methods: Retrospective chart review of HbSS patients in an outpatient pediatric hematology clinic was used to identify patients who had both TCDi and MRI performed between January 2018 to November 2023. Patients selected had a conditional TCDi (velocity >150 cm/s) or an abnormal MRI (infarct on MRI or stenosis on MRA). Those on chronic transfusion program were excluded. Logistic and linear regression models were used to assess the correlation between conditional TCDi and MRI and their relationship to Hb and bilirubin.
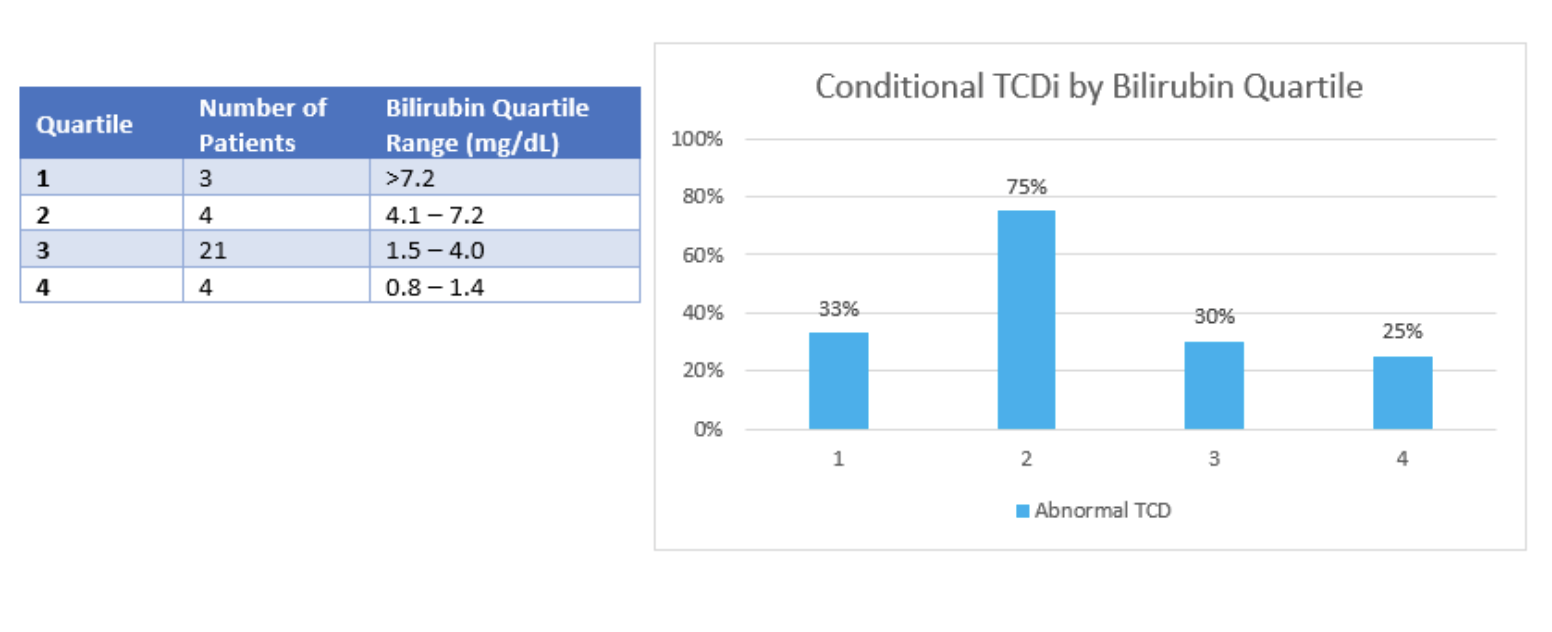
Results: A total of 32 patients were identified (Figure 1). Findings show that TCDi velocity is not a statistically significant predictor of an abnormal MRI (p=0.998). However, conditional TCDi velocity indicated a 1.9 times greater likelihood of an abnormal MRI. A lower baseline Hb and higher baseline bilirubin positively correlated with the likelihood of a conditional TCDi with 75% with a Hb between 5.7-7.7 g/dL (Figure 2) and 57.1% with bilirubin >4 mg/dl exhibiting abnormal TCDi (Figure 3).
Conclusion(s): Conditional TCDi did not correlate to abnormal MRI. Though not found to be statistically significant, it is 1.9 times more likely for a patient with a conditional TCDi to have an abnormal MRI. This may be related to other factors such as anemia, small versus large vessel disease or attenuation of the doppler. Despite the lack of correlation, TCDi remains the most specific predictor of primary stroke in sickle cell disease. There is a positive correlation between patients with lower levels of Hb and higher levels of bilirubin and the likelihood of a conditional TCDi. The pathophysiology of CNS disease in sickle cell is multifactorial It is likely a combination of effects of vaso-occlusion, hemolysis and inflammation. In this study, 65.6% of patients had conditional TCDi, supporting continued TCD screening. Our data suggests that screening for primary stroke risk and optimizing therapies is particularly important in patients with severe anemia and elevated bilirubin.
Figure 1. Results of TCD and MRI studies
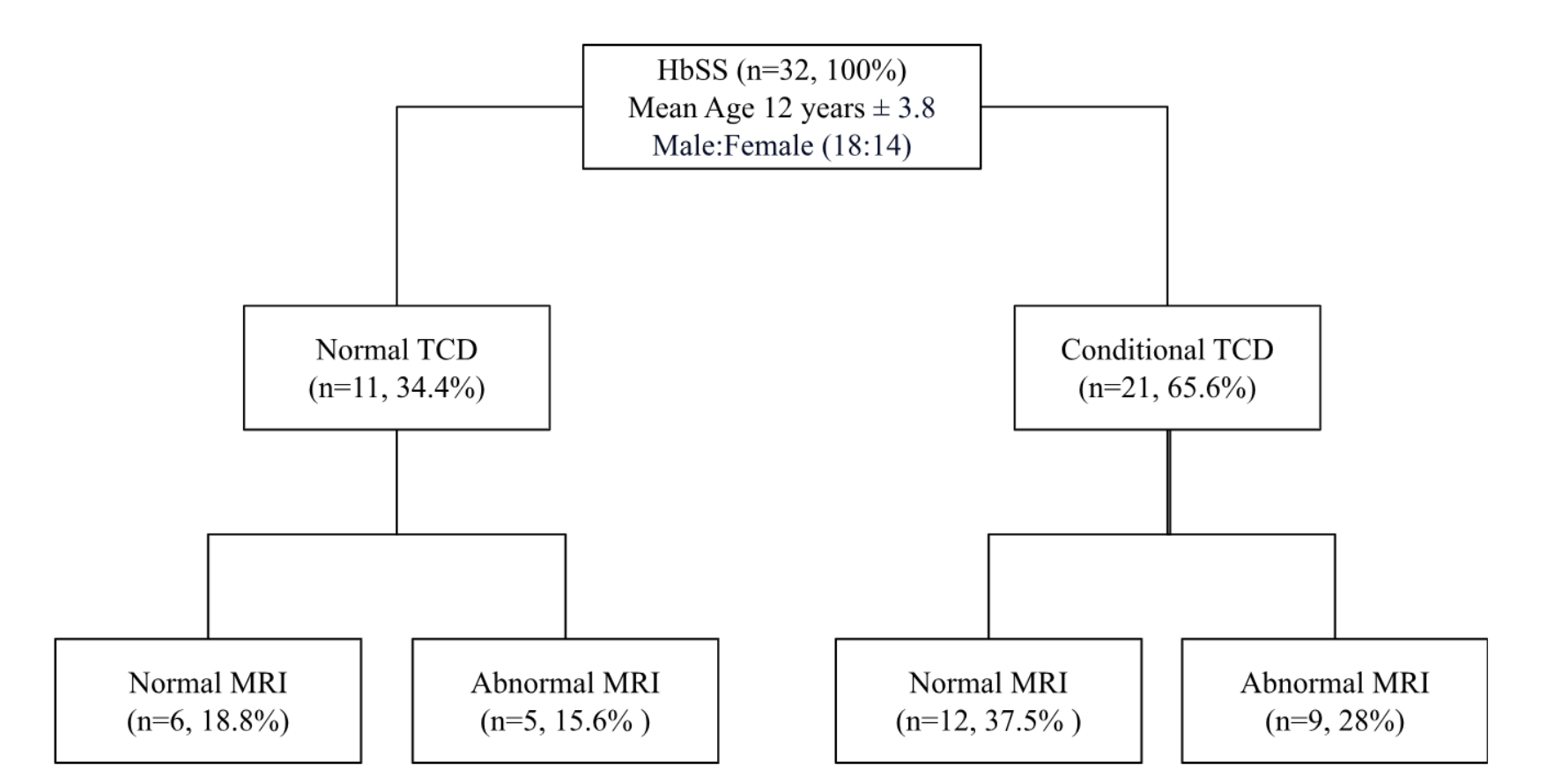
Figure 2. Conditional TCDi by Hemoglobin Quartiles
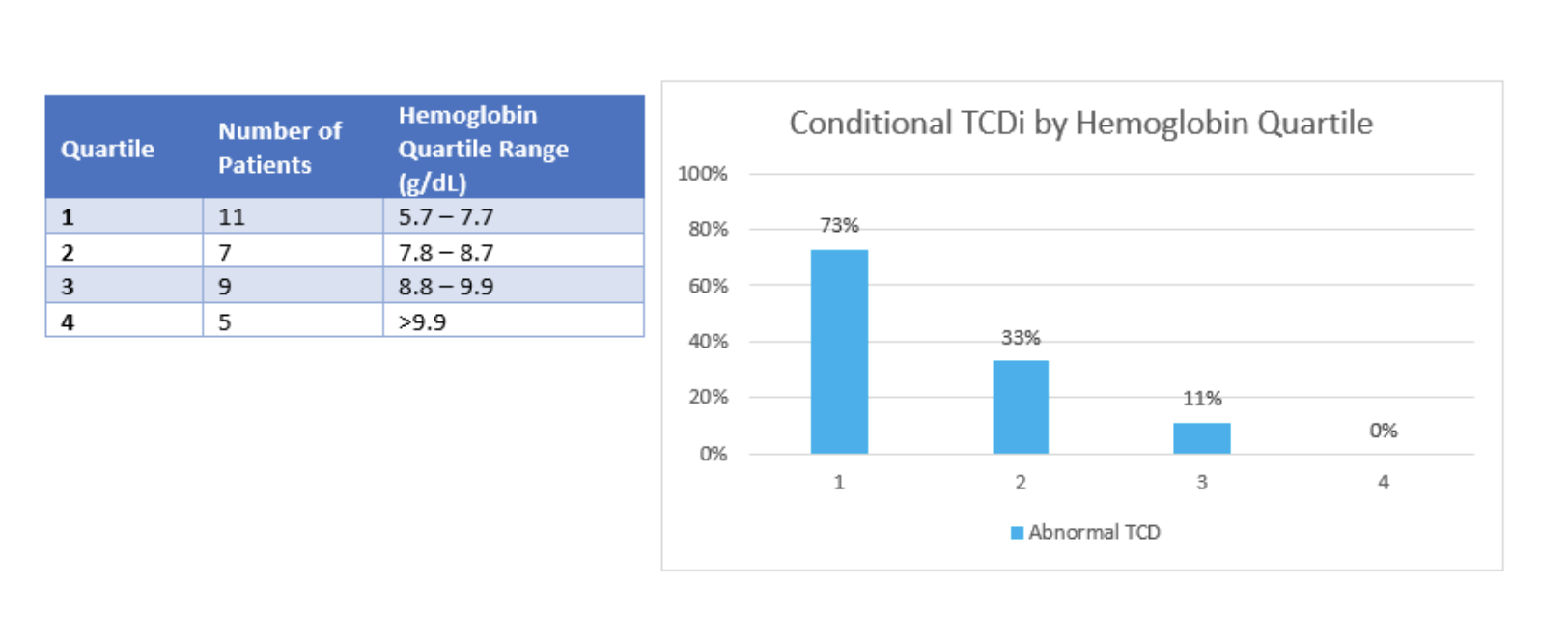
Figure 3. Conditional TCDi by Bilirubin Quartiles