Neonatal Quality Improvement 6
Session: Neonatal Quality Improvement 6
535 - Improving Direct Breastfeeding in a Level IV NICU
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 535.5283
Navin Bhopal, Phoenix Children's Hospital, Phoenix, AZ, United States; Michelle Weller, Phoenix Children's Hospital, Phoenix, AZ, United States; Bri Somerson, Phoenix Children's Hospital, Glendale, AZ, United States; Amy Brown, University of Arizona College of Medicine - Phoenix, Phoenix, AZ, United States; Shelley A. Akey, Phoenix Children's Hospital, Phoenix, AZ, United States; Abby Campbell, Phoenix Children's Hospital, Phoenix, AZ, United States; Jessica Chiang, Phoenix Children's Hospital, Phoenix, AZ, United States; Kristen Farnsworth, Phoenix Children's Hospital, Peoria, AZ, United States; Kimberlee Allred, Phoenix Children's Hospital, Phoenix, AZ, United States; Pamela Griffiths, Phoenix Children's Hospital, Phoenix, AZ, United States; Tara Kaleh, Phoenix Children's Hospital, Phoenix, AZ, United States; Sheralyn Kaprolet, Phoenix Children's Hospital, Phoenix, AZ, United States; Oleksandr Kudin, Phoenix Children’s Hospital, Phoenix, AZ, United States; Beth Larr, Phoenix Children's Hospital, Phoenix, AZ, United States; Jaclyn K. Rogowski, Phoenix Children's Hospital, Mesa, AZ, United States; Reece E. Englert, Phoenix Children's Hospital, Gilbert, AZ, United States; Deborah Tom, Phoenix Children's Hospital, Phoenix, AZ, United States; Jessica Wickland, Phoenix Children's Hospital, Phoenix, AZ, United States; Nisha Patel, Phoenix Children's, Phoenix, AZ, United States; Jacqueline Wyman, Phoenix Children's Hospital, Phoenix, AZ, United States; Jordan Teper, University of South Florida, Morsani College of Medicine, Tampa, FL, United States; Gregg Martin, Phoenix Children's Hospital, Cave Creek, AZ, United States
- NB
Navin Bhopal, MD
Neonatologist
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Human milk has a dose dependent effect on improving most neonatal morbidities and is an important quality metric in many NICUs. Due to various disease pathologies, many infants in the NICU initiate feedings via gavage tube with expressed breast milk. Historically, due to the need to quantify intake, infants in the NICU initiate PO feeding by bottle. Direct breastfeeding provides many benefits that are not conferred by feeding expressed milk via bottle, such as mother-infant bonding, improved neuro-regulation and more effective stimulation of maternal milk supply. Initiating direct breastfeeding in the NICU can help improve success of continued breastfeeding and milk supply post-NICU discharge. Our institution has been participating in the Children’s Hospital Neonatal Consortium (CHNC) Project Home QI project to improve human milk at discharge. We created an independent sub-project aiming to improve our direct breastfeeding rates for establishing the first PO feeds in a level IV NICU.
Objective: To increase the rates of first PO feedings at breast by 10% in 2 years from January 2023 to January 2025.
Design/Methods: QI Interventions:
• Early lactation education by IBCLCs and NICU physicians/APPs
• Development of milk milestones bedside tool (starting from oral care, progressing to skin-to-skin, non-nutritive breastfeeding and culminating in nutritive breastfeeding)
• Nursing education to improve comfort with breastfeeding, anticipate oral feeding readiness and engage mothers to be at bedside for first oral feeding
• Breastfeeding protocol to guide feeding tube supplementation
• Electronic order to promote first PO feeds at breast
• Protected 72hrs breastfeeding window whereby bottles are deferred in favor of direct breastfeeding
Results: The baseline rate of first PO feed at breast was 40%. In October, 2023, we introduced a PDSA cycle (Figure 1) to systematize direct breastfeeding. We saw improvement and a statistical shift by February 2024 (Figure 2). In September 2024, we altered our data collection method to improve accuracy.
Conclusion(s): Using a multidisciplinary approach involving physicians/APPs, lactation consultants, nursing and dietitians, we improved our direct breastfeeding rates in the NICU from 40% to approximately 95% in 21 months. We identified inconsistencies with data collection, which may have impacted our results, however despite this, our direct breastfeeding rates remain significantly improved from baseline. We hope this improvement will translate into improved breastfeeding and breast milk use rates post-NICU discharge.
Figure 1
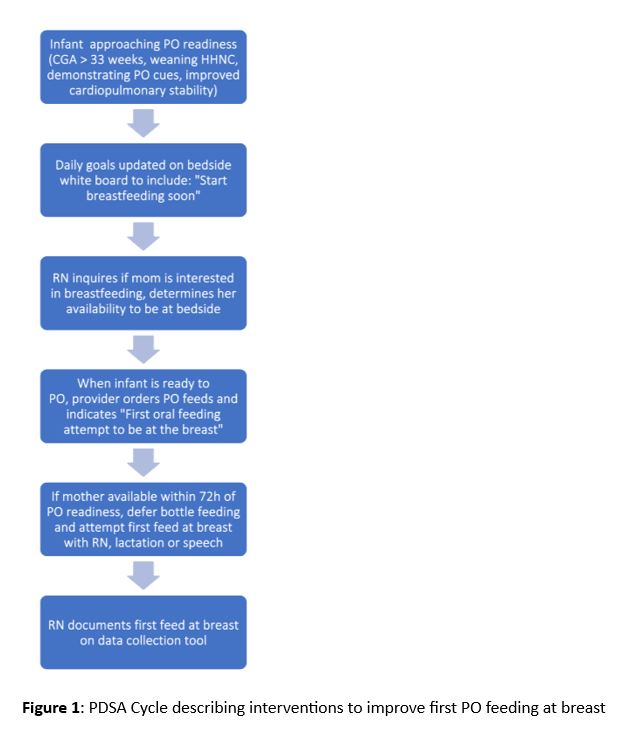 PDSA Cycle describing interventions to improve first PO feeding at breast
PDSA Cycle describing interventions to improve first PO feeding at breastFigure 2
.jpg) Run chart describing rates of first oral feeds at breast. The median rate of first oral feeds at breast was 40%. We introduced a systematic approach to first initiate the first PO feed at breast in November 2023 and saw a statistical shift in our breastfeeding rate starting in February 2024. In September 2024, we altered our data collection method to improve accuracy.
Run chart describing rates of first oral feeds at breast. The median rate of first oral feeds at breast was 40%. We introduced a systematic approach to first initiate the first PO feed at breast in November 2023 and saw a statistical shift in our breastfeeding rate starting in February 2024. In September 2024, we altered our data collection method to improve accuracy.

