Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
086 - Management of Bivalirudin for Primary Anticoagulation in Neonatal Respiratory ECMO Therapy within the Children’s Hospitals Neonatal Consortium
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 86.5707
Sandy Johng, Seattle Children's Hospital, Seattle, WA, United States; Robert DiGeronimo, Seattle Children's, Seattle, WA, United States; Mihai Puia-Dumitrescu, University of Washington School of Medicine, Seattle, WA, United States; Sarah Handley, University of Washington School of Medicine, Seattle, WA, United States; Zeenia Billimoria, University of Washington School of Medicine, Seattle, WA, United States; Katrin Lichtsinn, Seattle Children's, Seattle, WA, United States; Larissa A.. Yalon, Seattle Children's Hospital, Seattle, WA, United States; James Connelly, Children’s Hospital of Philadelphia, Philadelphia, PA, United States; Nicholas Carr, Intermountain Health, Sandy, UT, United States; Carly Heyrend, Primary Children's Hospital, Salt Lake City, UT, United States; Franscesca Miquel-Verges, University of Arkansas for Medical Sciences, Little Rock, AR, United States; David McCulley, University of California, San Diego School of Medicine, San Diego, CA, United States; Michelle Yang, University of Utah School of Medicine, Salt Lake City, UT, United States; Leslie Lusk, Benioff Children's Hospital Oakland, Oakland, CA, United States; Sharada H. Gowda, Baylor College of Medicine, Houston, TX, United States; Kelsey A.. Montgomery, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Natalie Rintoul, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Sandy Johng, MD (she/her/hers)
Assistant Professor of Pediatrics
Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Bivalirudin is a direct thrombin inhibitor that offers several advantages over heparin, which has been the anticoagulant of choice for extracorporeal membrane oxygenation (ECMO) for decades. Unlike heparin, bivalirudin can inhibit clot-bound thrombin and does not depend on antithrombin III, which is physiologically low in neonates. Its use has been increasingly adopted for pediatric patients undergoing treatment with ECMO. However, the absence of evidence-based guidelines results in varied practices regarding bivalirudin management, making standardization of care and assessment of efficacy challenging.
Objective: Our objective was to understand how bivalirudin is utilized for primary anticoagulation in neonatal respiratory ECMO therapy within the Children’s Hospitals Neonatal Consortium (CHNC).
Design/Methods: We developed an ECMO anticoagulation RedCap survey that underwent pretesting and pilot testing by multi-center experts in the field – including neonatologists, ECMO coordinators, and an anticoagulation pharmacist – who evaluated the face and content validity of the survey. Centers reporting bivalirudin as their primary anticoagulant were asked additional questions regarding its management. The survey was distributed to members of the CHNC ECMO Focus Group from April to May 2024. Results were summarized using counts and proportions.
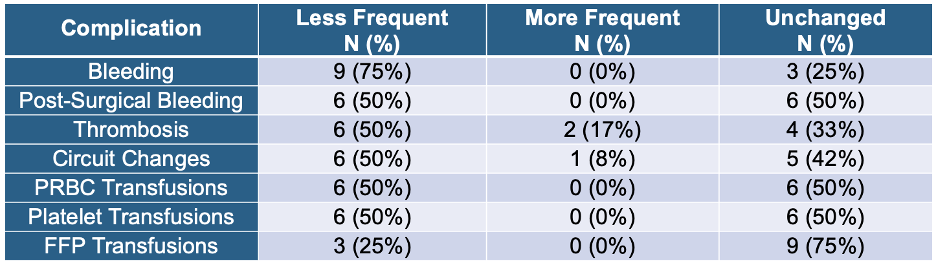
Results: We received 39 responses from 32/37 (86%) centers. Among these, 10/32 (31%) identified bivalirudin as their primary anticoagulant, with 4/10 (40%) being high-volume centers managing over 10 neonatal respiratory ECMO cases annually. All transitioned to bivalirudin within the past 5 years. Bivalirudin management practices varied across these centers (Figure 1). Among the 12 respondents who primarily use bivalirudin, the consensus was that bleeding and clotting complications had decreased compared to heparin (Table 1).
Conclusion(s): Despite growing interest in using bivalirudin for anticoagulation in neonatal respiratory ECMO, a minority of centers have adopted it as their primary anticoagulant. Among these centers, there is considerable variation in how bivalirudin is managed. Although this survey demonstrates the perception that complications related to hemostasis were less frequent after the implementation of bivalirudin-based anticoagulation, it will be important to demonstrate this finding in a clinical research study. There is a critical need and opportunity to standardize management practices to accurately investigate the advantages, disadvantages, and optimal administration methods for bivalirudin therapy in neonatal ECMO treatment.
Figure 1: Comparative chart of bivalirudin management among CHNC centers using bivalirudin as the primary anticoagulant for neonatal respiratory ECMO.
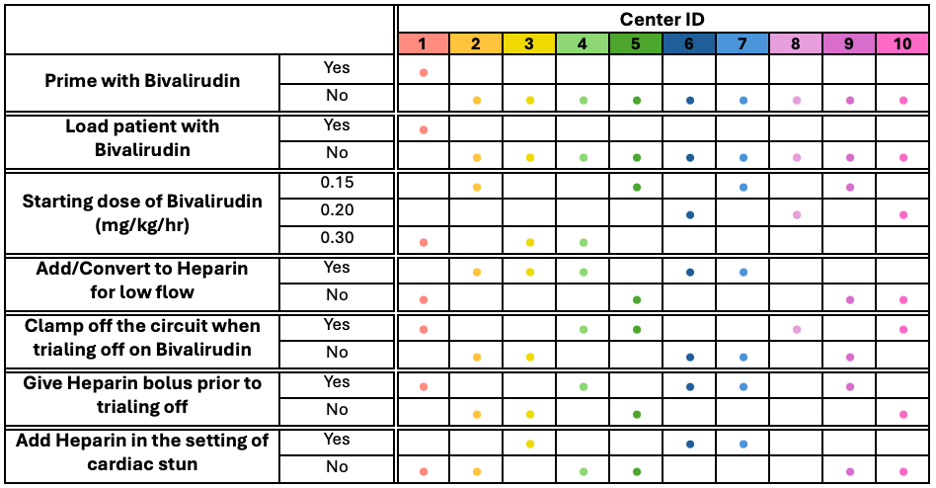
Table 1: Survey respondent impressions on frequency of complications with bivalirudin compared to heparin for primary anticoagulant type in neonatal respiratory ECMO therapy.