Neonatal Hemodynamics and Cardiovascular Medicine 2
Session: Neonatal Hemodynamics and Cardiovascular Medicine 2
056 - Outcomes and Follow-Up of Extremely Preterm Infants with a Severe Cardiovascular Profile Secondary to a Hemodynamically Significant Patent Ductus Arteriosus
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 56.5663
Kaitlyn Miller, Nationwide Children's Hospital, Columbus, OH, United States; Carl Backes, Nationwide Children's Hospital, Col, OH, United States; Clifford L. Cua, Nationwide Children's Hospital, Columbus, OH, United States; Brian Rivera, The Abigail Wexner Research Institute at Nationwide Children's Hospital, Columbus, OH, United States; Sara Conroy, Nationwide Children's Hospital, Columbus, OH, United States
.jpg)
Kaitlyn Miller, MD (she/her/hers)
Neonatology Fellow
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Treatment and management of extremely preterm infants (EPIs) with a hemodynamically significant patent ductus arteriosus (HSPDA) remains controversial. In a conservative, non-interventional approach, the HSPDA is not procedurally closed; the infant’s prematurity is managed, and healthcare providers closely monitor the symptomatic PDA, while awaiting the possibility of spontaneous closure. Despite widespread acceptance, this approach potentially increases the risk of developing severe cardiovascular consequences due to the HSPDA. Outcomes and follow-up of this population are not well defined.
Objective: To evaluate the outcomes and follow-up practices of EPIs who develop a severe CV profile secondary to their HSPDA.
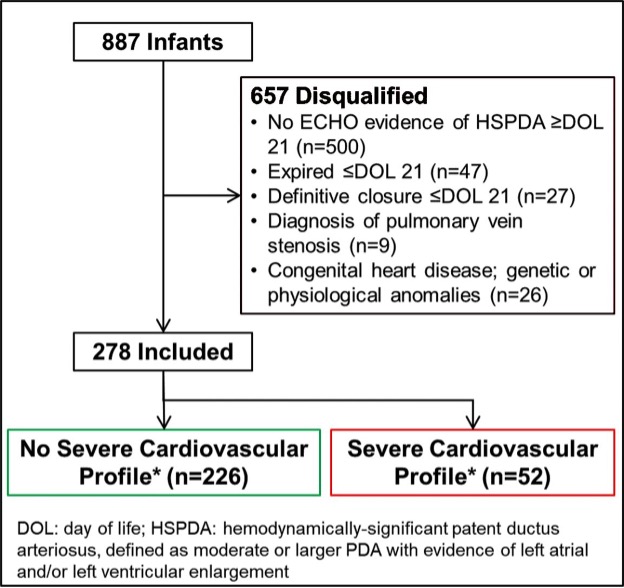
Design/Methods: Contemporary (1/2010-12/2019), retrospective review at a large, pediatric referral center. The cohort included EPIs with HSPDA > postnatal day 21 (beyond window when drug therapy is most efficacious). HSPDA was defined by both echocardiographic (moderate/large ductus based on minimum diameter and left-sided atrial/ventricular chamber enlargement) and clinical (need for mechanical ventilation) criteria. Severe cardiovascular compromise was defined as left-sided cardiac enlargement (Z-score > 4) with damage to the mitral valve apparatus (e.g., mitral regurgitation) clearly/likely attributable to HSPDA exposure (absence of other etiologies).
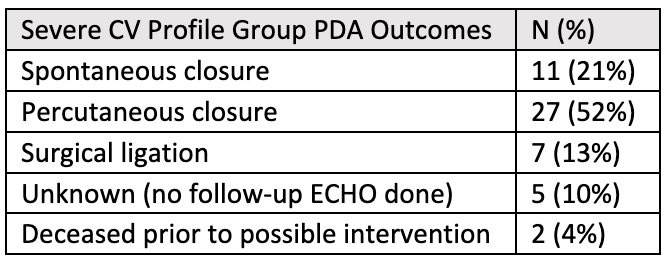
Results: Among 278 EPIs with HSPDA, 803 ECHOs were independently reviewed; 52 infants (19%) had severe cardiovascular compromise. Of the severe CV profile group, there were 34 infants (65%) who failed conservative treatment and underwent procedural closure (7 surgical ligations, 27 percutaneous). The remaining 18 (35%) infants had spontaneous ductal closure (21%), no follow-up ECHO available for review (10%), or had expired prior to potential intervention (4%). Most patients (92%) survived to initial hospital discharge. There were 2 patients (3.8%) that continued to have significant mitral regurgitation discharged home on an ACE-inhibitor. There were 25 patients (48%) who were seen by cardiology due to their severe CV profile after NICU discharge.
Conclusion(s): Optimal management strategies for EPIs with an HSPDA remain unanswered, reinforcing the critical need for well-designed, pragmatic clinical trials in this high-risk subgroup. As conservative management has become more common, it is likely that more patients will develop a severe CV profile. It would be useful to evaluate other centers’ outcomes and follow-up of this vulnerable subgroup of EPIs to create standardized guidelines.
Flow Diagram of Severe Cardiovascular Profile Group
Outcomes of Patients with Severe CV Profile
Number of Cardiology Visits Related to History of Severe CV Profile
.jpg)

