Neonatal Quality Improvement 5
Session: Neonatal Quality Improvement 5
517 - Improving Time Spent at Target Oxygen Saturations in Very Low Birth Weight Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 517.5208
Darah Yuhas, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; Oscar G. Winners-Mendizabal, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; Joana Machry, Johns Hopkins All Children's Hospital, SAINT PETERSBURG, FL, United States

Darah Yuhas, MD (she/her/hers)
Neonatal-Perinatal Fellow
Johns Hopkins All Children's Hospital
Tampa, Florida, United States
Presenting Author(s)
Background: The mean annual incidence of severe retinopathy of prematurity (ROP) in VLBW infants at the Johns Hopkins All Children’s (JHACH) NICU is 11.7% compared to the national average of 8% for comparable NICUs. Hyperoxia (SpO2 >95%) leads to an increased rate of ROP and adverse pulmonary effects, while hypoxia (SpO2 < 90%) has shown to increase mortality and necrotizing enterocolitis. Despite the known importance of targeting a narrow oxygen saturation range, in the JHACH NICU, VLBW infant’s oxygen saturations are only within the goal range of 90-95% 44 percent of the time.
Objective: The aim was to increase the time spent in target range oxygen saturation (SpO2 90-95%) from 42% to 65% in VLBW infants by December 2024. The Global aim was to decrease the mean annual incidence of severe ROP in VLBW infants from 11.7% to 8%.
Design/Methods: A survey was distributed to establish baseline knowledge of target oxygen goals and histograms (Tab 1). Based on identified barriers, a key driver diagram was created (Fig 1). The outcome measure was the average percent of time spent at goal oxygen saturation. Process measures included number of patients with histogram data documented in the EMR and percent of correct bedside alarm parameters. Balancing measures included percent of time spent below target oxygen saturation range and BPD and ROP rates. Infants were included if birth weight was < 1500g and required oxygen. They were excluded if diagnosed with pulmonary hypertension or cyanotic congenital heart disease. Data analysis was conducted via statistical process control charts created in Microsoft Excel with QI Macros.
Results: Time spent at goal oxygen saturations increased from a mean of 44.2% to 60.9% (Fig 2). Percent of correct alarm limits increased from a mean of 65% to 86% (Fig 3). Histograms were documented in the EMR 75% of the time during the first month of implementation and increased to 88%. Special cause variation was noted in the outcome and process measures. For the balancing measures, the time spent below goal oxygen saturations did not significantly differ over time and there was no significant difference in the annual rate of NEC or BPD.
Conclusion(s): We successfully increased the time VLBW infants spent at the target oxygen saturation range. The interventions we introduced led to routine use of histogram data during rounds, handoff and bedside assessments, which we believe led to the improvement in our primary outcome. The mean annual incidence of ROP also decreased from 11.7% to 7.7%. We believe the efforts of this quality improvement initiative contributed to the improvement in ROP in our NICU.
Key Driver Diagram
.png) Key driver diagram for increasing time spent at goal oxygen saturation, linking change ideas to primary drivers.
Key driver diagram for increasing time spent at goal oxygen saturation, linking change ideas to primary drivers.Time spent at Target Oxygen Saturation Control Chart
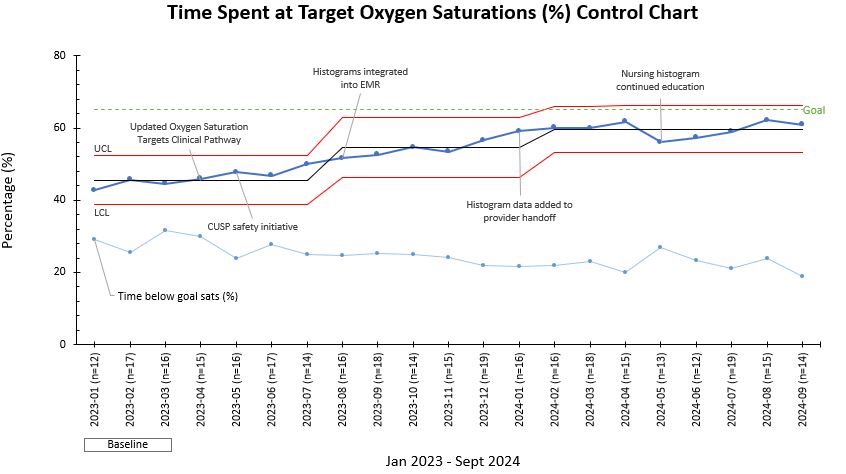 Control chart displaying average monthly time spent at goal oxygen saturation in VLBW infants requiring oxygen from January 2023
Control chart displaying average monthly time spent at goal oxygen saturation in VLBW infants requiring oxygen from January 2023 through September 2024. Interventions are annotated. Center line (mean) was adjusted after special cause variation was noted. Red lines indicate the upper control limit and lower control limit.
Process Measure Control Charts
.jpg) A, Control chart displaying average monthly alarm limits set accurately in VLBW infants requiring oxygen from January 2023 through September 2024. Red lines indicate the upper control limit and lower control limit. The center line (mean) was adjusted after special
A, Control chart displaying average monthly alarm limits set accurately in VLBW infants requiring oxygen from January 2023 through September 2024. Red lines indicate the upper control limit and lower control limit. The center line (mean) was adjusted after specialcause variation was noted. B, Control chart displaying average monthly histogram EMR documentation in VLBW infants requiring oxygen from August 2023 through September 2024. Red lines indicate the upper control limit and lower control limit. The center line (mean) was adjusted after special cause variation was noted.


