Medical Education 3: Simulation
Session: Medical Education 3: Simulation
208 - Implementing a Multidisciplinary Trauma Simulation Curriculum for Pediatric Emergency Medicine Fellows
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 208.5222
Carissa Bunke, Children's Hospitals and Clinics of Minnesota, Inver Grove Heights, MN, United States; Heather A. Hartman, Nemours Children's Hospital, Wilmington, DE, United States; Alisha Ching, University of Michigan Medical School, Ann Arbor, MI, United States; Timothy Visclosky, University of Michigan Medical School, Ann Arbor, MI, United States

Carissa Bunke, MD (she/her/hers)
Pediatric Emergency Medicine Faculty
Children's Hospitals and Clinics of Minnesota
Inver Grove Heights, Minnesota, United States
Presenting Author(s)
Background: Unintentional injury is a leading cause of morbidity and mortality in children. Approximately 8 million injured pediatric patients present to Emergency Departments (ED) each year. Accordingly, the Accreditation Council for Graduate Medical Education (ACGME) requires competency in medical and trauma resuscitations in patients from newborn through adulthood. Yet there is a paucity of data regarding best practices for pediatric trauma training.
Objective: To evaluate knowledge gaps in pediatric trauma training, implement a trauma simulation curriculum, and evaluate changes in fellows comfort level with trauma skills pre- and post-implementation.
Design/Methods: We utilized Kern’s six-step approach to design a longitudinal trauma curriculum for Pediatric Emergency Medicine (PEM) fellows. A multidisciplinary team performed a needs assessment of PEM faculty, PEM fellows, pediatric surgery faculty, pediatric surgery fellows, and pediatric ED nursing. Learning objectives were categorized in the domains of technical skills, non-technical skills, and case-based medical knowledge. This guided the development of a year-long curriculum with 11 simulation cases and three didactic sessions (Table 1).
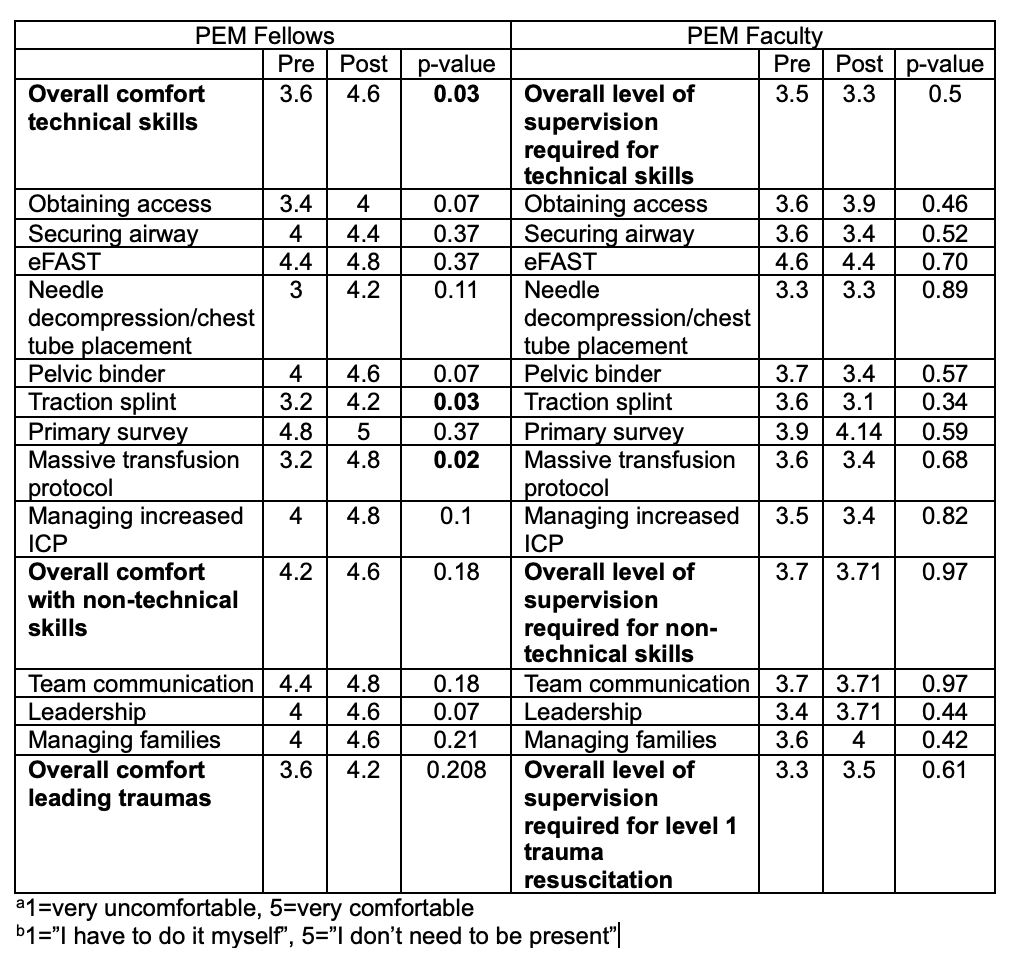
The curriculum was assessed at Kirkpatrick levels one and two using pre- and post-implementation surveys. Surveys assessed PEM fellows self-reported comfort and PEM faculty perception of the level of supervision fellows required. Pre- and post-implementation surveys were compared using a paired t-test.
Results: Survey results are shown in Figure 2. Fellows began with higher overall comfort with non-technical skills compared to technical skills. Pre- and post-implementation comparison demonstrated a significant improvement in fellow comfort in overall technical skills, traction splint application, and initiating massive transfusion protocol. There were trends toward improvement, though not significant, in obtaining access, placing pelvic binders, managing increased intracranial pressure, and leadership skills. Fellows gave positive feedback particularly on the technical skills aspects of the curriculum. There were no significant findings in the faculty surveys.
Conclusion(s): This study presents a promising foundation for a comprehensive longitudinal pediatric trauma curriculum. Our study, while small, showed overall improvement in fellow comfort with trauma resuscitations at Kirkpatrick level one, most notably with technical skills. Future areas of research include increased sample size, enhanced skills assessment methods, and expansion to other trauma team stakeholders.
Figure 1: PEM Fellows Pre and Post Survey Results
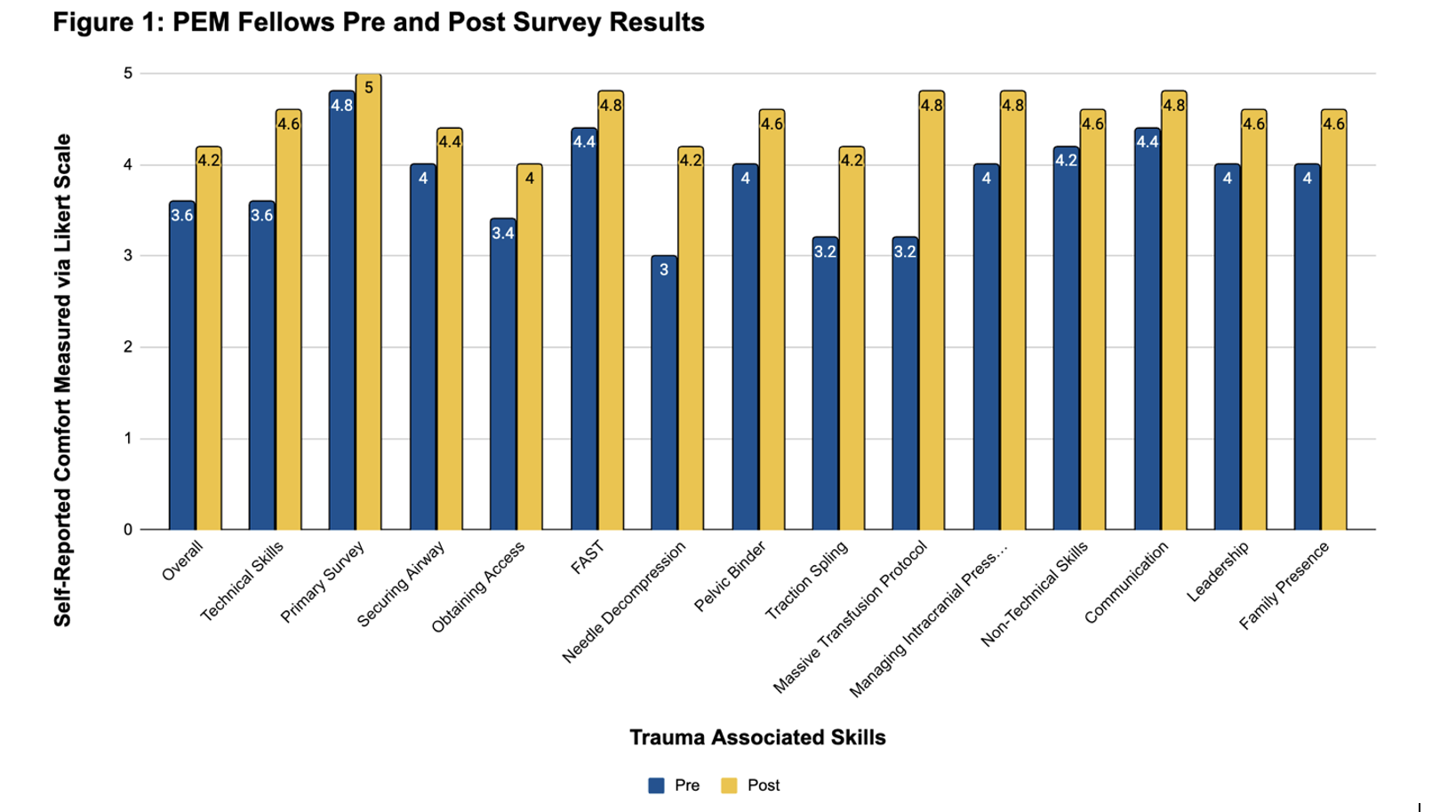 Results of PEM Fellows pre and post-implementation survey. Fellows rated their self-reported comfort in various aspects of trauma resuscitations on a Likert scale. Results were averaged and compared via a paired T-test. There was statistically significant improvement (p <0.05) in overall technical skills, traction splint application, and initiating massive transfusion protocol.
Results of PEM Fellows pre and post-implementation survey. Fellows rated their self-reported comfort in various aspects of trauma resuscitations on a Likert scale. Results were averaged and compared via a paired T-test. There was statistically significant improvement (p <0.05) in overall technical skills, traction splint application, and initiating massive transfusion protocol.Table 1: Trauma simulation curriculum blueprint