Medical Education 5: Procedures and Simulation
Session: Medical Education 5: Procedures and Simulation
231 - Impact of a Pediatric Residency Bootcamp on Clinical and Procedural Skill Development: Post-Residency Improvements Following Participation in a Pre-Graduation Bootcamp
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 231.5262
Mahati Pidaparti, Indiana University School of Medicine, Indianapolis, IN, United States; Priya G. Jain, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Karen Mangold, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States

Mahati Pidaparti, MD
Fellow
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Because pediatric residencies focus on training residents broadly, residents may graduate without exposure to a full depth of experiences in their chosen future careers.
Objective: Three career-specific bootcamps were developed based on a needs assessment of pediatric residency graduates, and the usefulness was further evaluated with post-graduation surveys.
Design/Methods: An anonymous survey was distributed in May 2021 to all categorical pediatric graduating/graduated residents from 2017-2021 regarding skills they wished they had obtained prior to graduation. The survey was used to develop career-specific pediatric residency bootcamps (critical care, outpatient, and research) held at the end of the 3rd year of residency in 2022 and 2023 to focus on skills that graduates feel are both important to know and inadequately covered during residency. Anonymous surveys were administered in April 2024 to graduated residents from 2022 and 2023 to evaluate the usefulness of the bootcamps. Parametric testing measured distribution of clinical variables.
Results: 67 residency graduates completed the needs assessment survey. There were differences based on career path in graduates’ perception of importance in future career and desire for more practice with certain skills/procedures during residency (Table 1). A total of 37 residents participated in a bootcamp in 2022 and 2023, with 19 in critical care, 10 in outpatient and 9 in research tracks. Of the 21 post-bootcamp survey participants, most residents who participated in the critical care (n=10) or research (n=3) tracks felt that it was very or extremely helpful, however those who participated in the outpatient track (n=2) did not find it as helpful. The average confidence in most skills practiced during each of the tracks (critical care: bag-mask ventilation, intubation, umbilical line placement, peripheral intravenous catheter placement; outpatient: billing, ICD coding, documentation of risk/errors; research: IRB procedures, statistical analysis) were higher in those who attended the bootcamp compared to the pre-survey respondents (Table 2).
Conclusion(s): Although pre-bootcamp confidence in various skills was not strongly correlated with post-residency career paths, the differences in perceived importance of certain skills for future careers, along with the desire for more practice during residency, highlight the need for career-specific bootcamps prior to graduation. While there was improvement in confidence in skills post-bootcamp, more work needs to be done to develop bootcamps that are not just procedure-based but also helpful for non-procedural careers.
Table 1: Needs Assessment Survey Results of Graduated Pediatric Residents
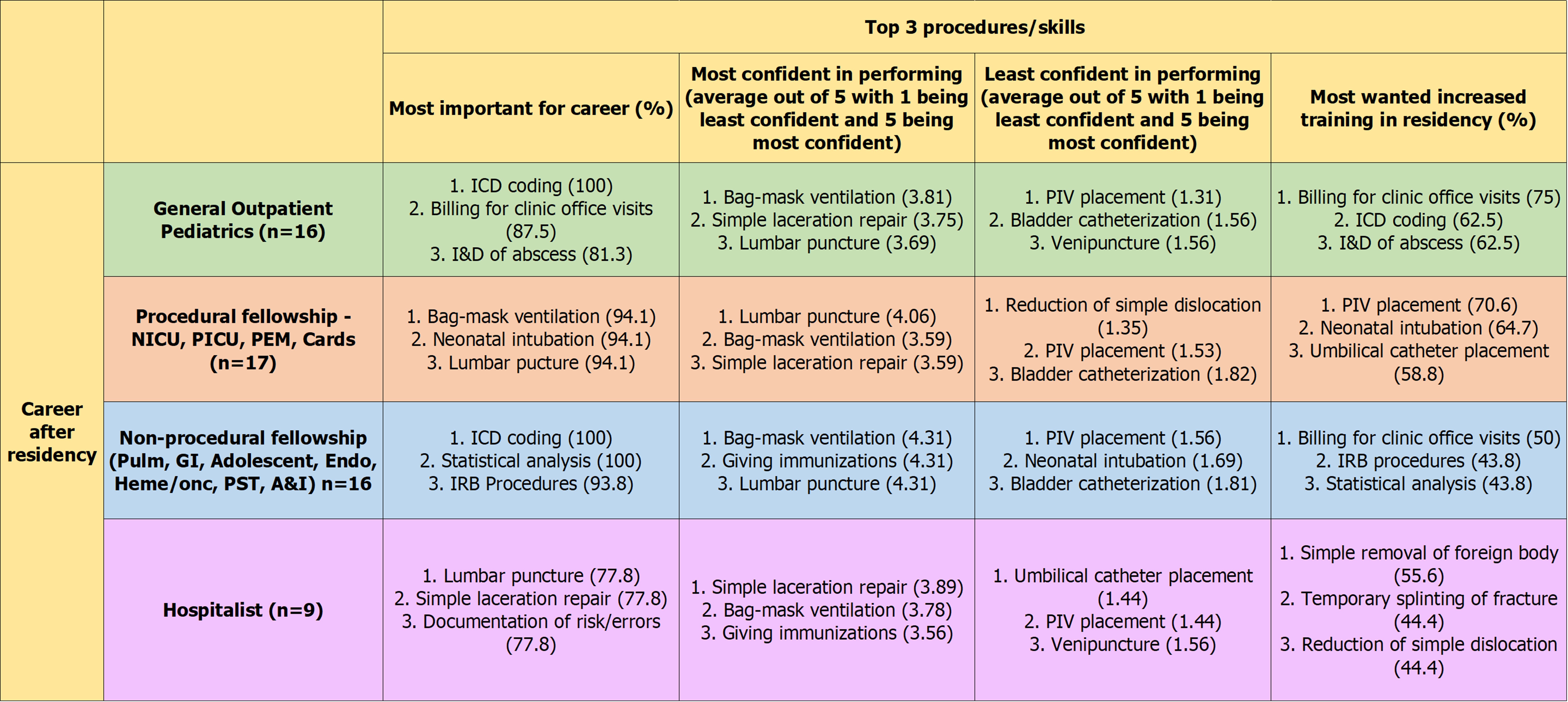 Needs assessment table showing graduated residents’ perception of the most important skills, the skills they feel most and least confident in, and the skills they desired the most increased training in residency.
Needs assessment table showing graduated residents’ perception of the most important skills, the skills they feel most and least confident in, and the skills they desired the most increased training in residency.Table 2: Post-bootcamp Survey Results in Confidence of Skills
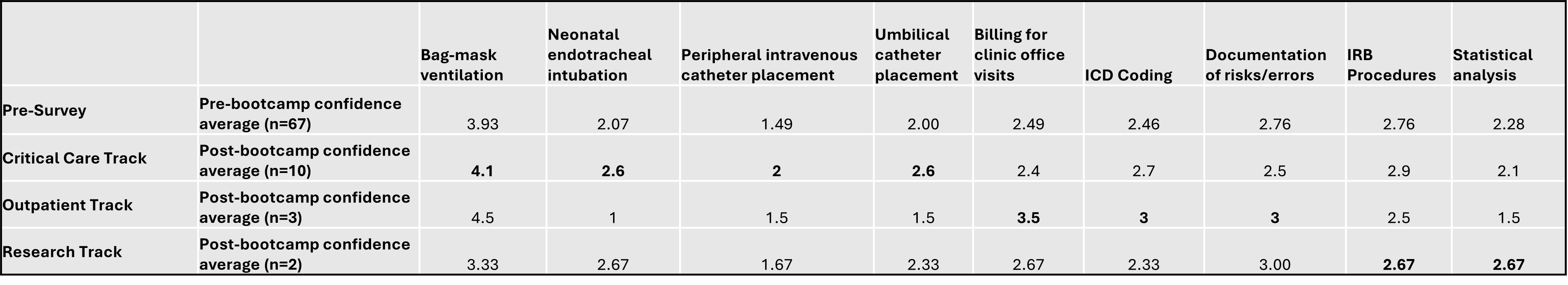 Post-bootcamp survey results showing the differences in average confidence in skills. Each value is average out of 5 with 1 being least confident and 5 being most confident. Bolded values are the skills that were taught and practiced during the career-specific bootcamps based on the needs assessment survey results.
Post-bootcamp survey results showing the differences in average confidence in skills. Each value is average out of 5 with 1 being least confident and 5 being most confident. Bolded values are the skills that were taught and practiced during the career-specific bootcamps based on the needs assessment survey results.
