Medical Education 3: Simulation
Session: Medical Education 3: Simulation
198 - “My body thinks this is real”: Fourth Year Medical Student Perspectives of a Simulated Pediatric Inpatient Experience
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 198.3872
Jennifer A. McConnell, University of Texas Southwestern Medical School, Dallas, TX, United States; Cameron Wynn, University of Texas Southwestern Medical School, Dallas, TX, United States; Ailyn Clara, UT Southwestern, Dallas, TX, United States; Prachi Singh, UTSW, Dallas, TX, United States; Jeanne Carey, UT Southwestern Medical Center, Dallas, TX, United States; Rory Nicolaides, University of Texas Southwestern Medical Center, Dallas, TX, United States; Ngoc Van Horn, University of Texas Southwestern Medical School, Dallas, TX, United States; Jenny KR. Francis, University of Texas Southwestern Medical Center, Dallas, TX, United States
- JM
Jennifer A. McConnell, MD (she/her/hers)
Fellow
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Since 2019, a pediatric inpatient simulation for pediatrics-bound fourth-year medical students consistently provoked reactions of realism and positive feedback. We used qualitative methods to describe student perspectives of the simulation.
Objective: Describe graduating medical students’ perspectives of learning in a pediatric inpatient simulation to characterize components of a realistic simulation-based learning experience.
Design/Methods: Twenty-five fourth year medical students matched to Pediatrics or Combined Internal Medicine-Pediatrics participated in a pediatric inpatient simulation during the annual transitions-to-residency course in March 2024. During the 90-minute simulation, 5 teams of 5 students received a simulated hand-off, managed interruptions, and addressed patient deteriorations with embedded distractions, to practice future roles, teamwork, communication and escalation of care. We invited students to virtual semi-structured interviews within one month of the simulation until we reached saturation. We transcribed interviews verbatim. Four independent coders followed a thematic framework with inductive and deductive approaches for analysis where consensus resolved discordance.
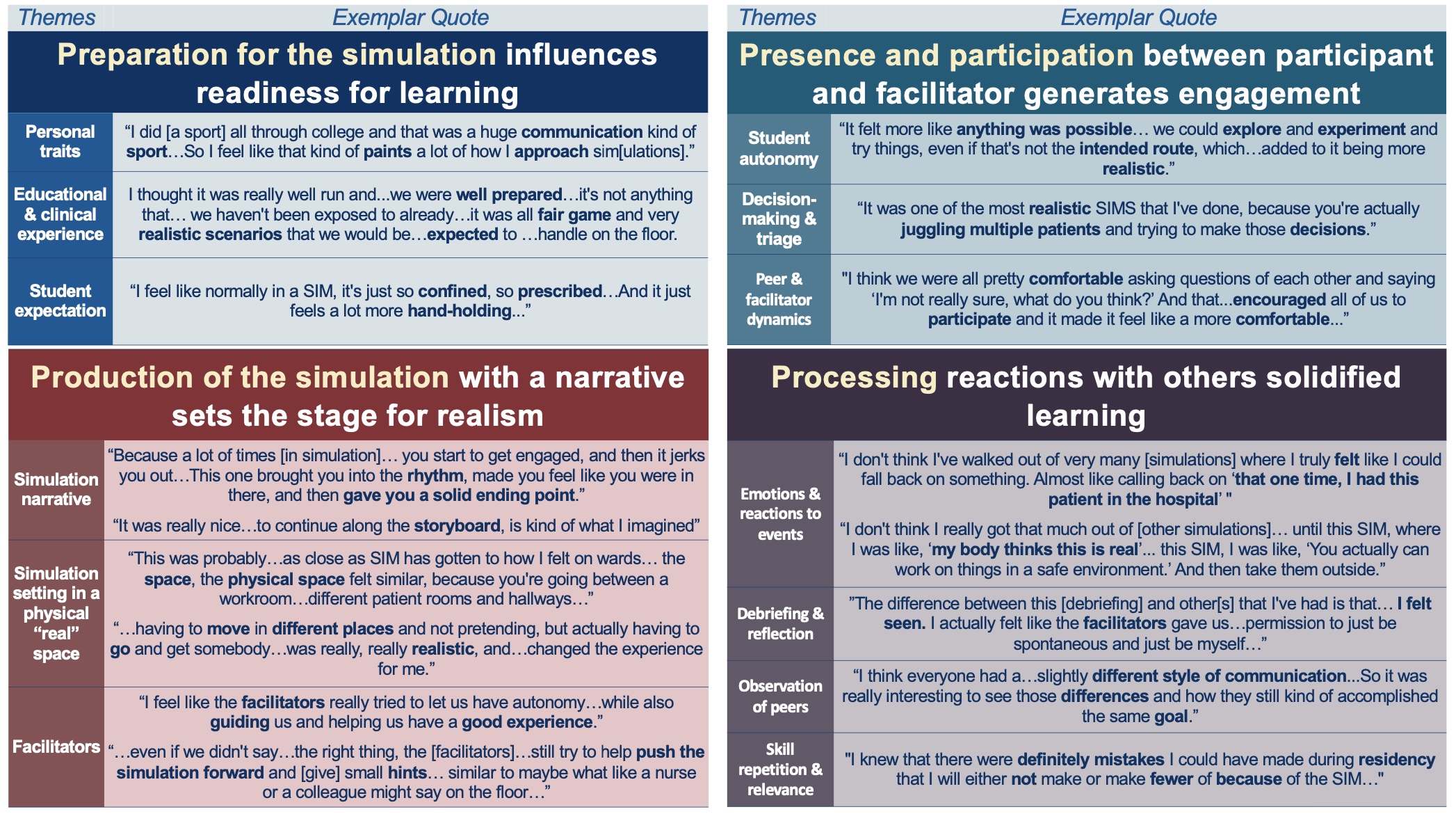
Results: Most interviewees (80%, n=20/25) gave virtual interviews (18/20 individual, 2/20 combined), were female (70%), matched to Pediatrics (85%), aged 25–34 years, and interviewed between 4–20 days post-event, for 30–59 minutes (average 41 minutes). We found four main themes. First, preparation: personal, educational, and clinical experience influenced expectations. Second, production: a narrative structure, including interruptions and deteriorations, was generated by facilitators and equipment within a multi-room “real space.” Third, presence: autonomy, decision-making, and interactions with peers and facilitators drove engagement and realism (one student said: “My body felt this is real”). Fourth, processing: debriefing and reflection of emotions and reactions, peer observation, skill repetition, and relevance to future practice enhanced learning. As one student said: “I truly felt like I could fall back on something. Almost like calling back on, ‘That one time, I had this patient’.”
Conclusion(s): The concepts of preparation for the simulation, production and delivery of the simulation narrative, the presence of students, and processing to solidify learning are the key features described by students in this study. Future studies should investigate how the balance of student autonomy, narrative structure, and facilitator roles within a real space strengthens simulation realism.
Themes and Quotes