Health Equity/Social Determinants of Health 9
Session: Health Equity/Social Determinants of Health 9
192 - Structural Racism and Parents’ Perceptions of Care Access, Quality, and Experiences in Pediatric Clinics
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 192.6983
Nita Vangeepuram, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Radhi Yagnik, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Lobsang Palmo, Columbia University, JACKSON HEIGHTS, NY, United States; Lauren Gordon, Icahn School of Medicine at Mount Sinai, New York, NY, United States; Jennifer Hong, State University of New York Downstate Medical Center College of Medicine, Brooklyn, NY, United States; Lynne D. D.. Richardson MD, Mount Sinai Health System, New York, NY, United States; Carol R. Horowitz, Icahn School of Medicine at Mount Sinai, NYC, NY, United States; Nina Bickell, Icahn School of Medicine at Mount Sinai, New York, NY, United States

Nita Vangeepuram, MD, MPH (she/her/hers)
Associate Professor
Icahn School of Medicine at Mount Sinai
New York, New York, United States
Presenting Author(s)
Background: Structural racism persists in healthcare and may affect patient care quality and experiences in clinics with varying levels of segregation of care by insurance and race/ethnicity. There is, however, surprisingly little research on the impact of segregated healthcare on parents’ perspectives about pediatric care delivery and quality.
Objective: We aimed to identify practices with varying levels of segregation by insurance and race/ethnicity and examine parents’ perceptions of care access, quality and experiences in more and less segregated pediatric practices.
Design/Methods: We identified pediatric clinics from a large urban health system with varying levels of segregation based on composite scores calculated from the distribution of patients by insurance and race/ethnicity. We identified 3 clinics: most segregated and advantaged (Clinic A); most segregated and disadvantaged (Clinic B); and most unified (Clinic C). We randomly sampled and surveyed ~60 parents/caregivers per clinic and examined differences in outcomes of interest using chi square and one-way ANOVA tests.
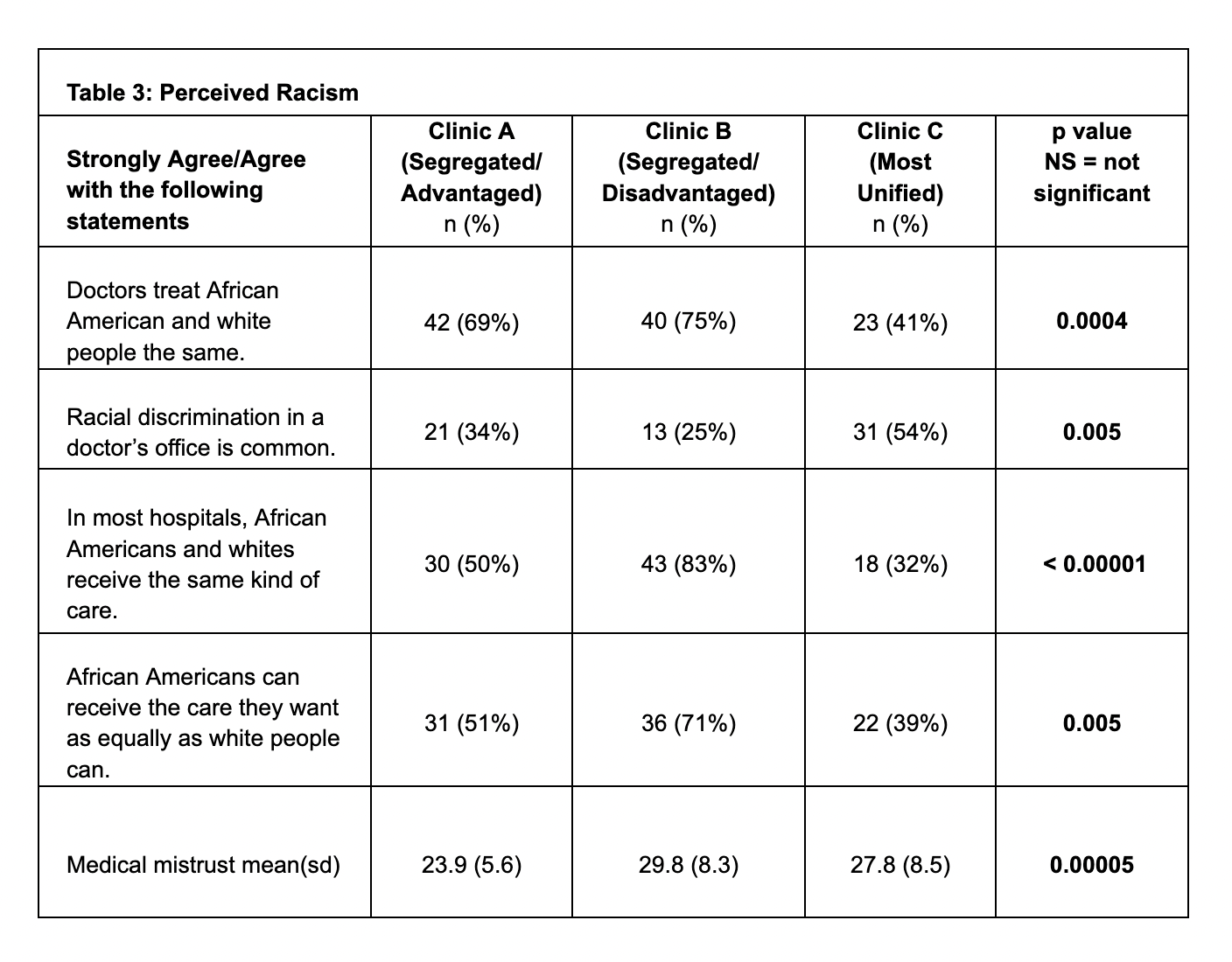
Results: Clinics A, B, and C varied by race/ethnicity (58%, 4%, and 27% White, respectively, p< 0.00001) and Medicaid insurance (0%, 72%, and 25% respectively, p< 0.00001). Table 1 includes additional demographic characteristics. Parents reporting that they can usually, almost always, or always access routine care and get answers to medical questions did not vary across practices. However, access to urgent care was lower in Clinic B (Table 2). There were few differences across the clinics in parents’ perceived care including overall positive feedback about treatment by staff; doctors’ knowledge of their patients, quality of communication, and doctors’ attributes (i.e., listening, being respectful, spending enough time). Clinic B parents reported longer wait times (Table 2). Clinic C parents were most likely and Clinic B parents were least likely to perceive racism towards Blacks in healthcare settings. Medical mistrust (score range 12-60) was higher in Clinics B and C than Clinic A; p=0.00005).
Conclusion(s): Parents’ perceived access to and quality of care was generally similar across pediatric clinics with varying levels of segregation by insurance and race/ethnicity. However, access to urgent care and wait times were worse in the segregated/disadvantaged clinic. Interestingly, perceived racism and medical mistrust were more prevalent in the most unified and diverse practice; further research is needed to explore reasons for these differences.
TABLE 1: Clinic Demographic Characteristics
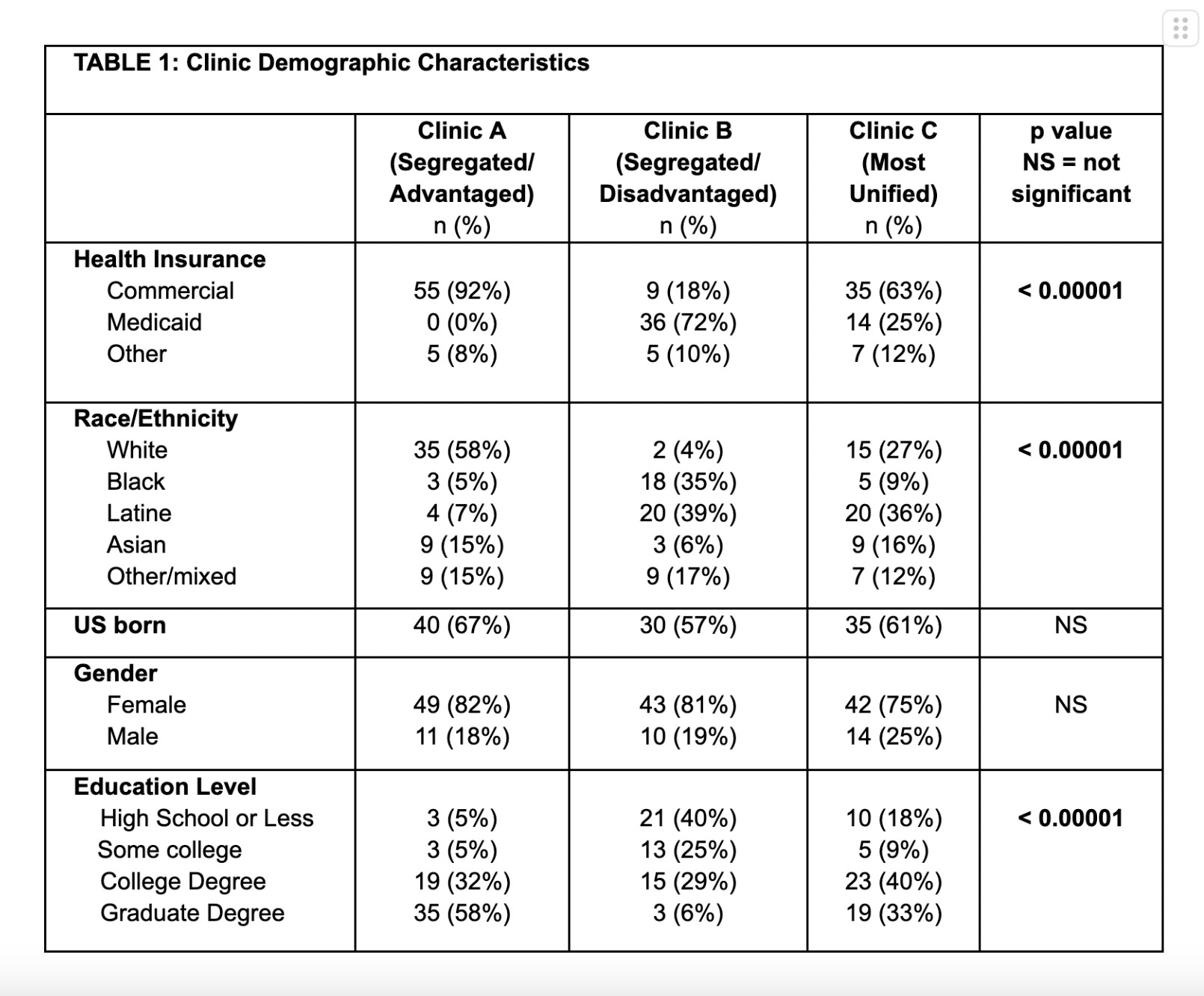
TABLE 2: Access to and Experiences of Care
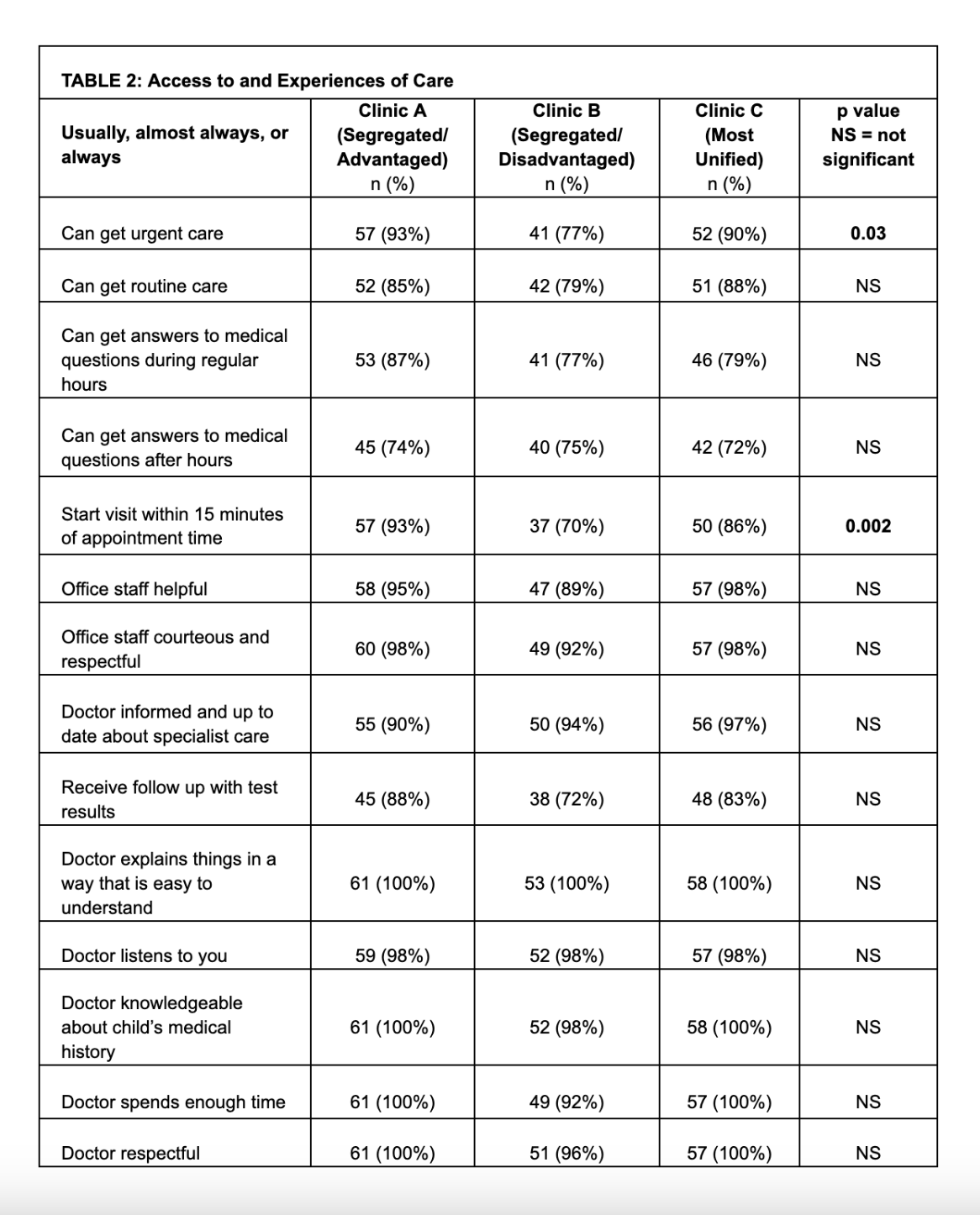
Table 3: Perceived Racism