Neonatal/Infant Resuscitation 4
Session: Neonatal/Infant Resuscitation 4
403 - Debriefing Newborn Resuscitation and Stabilization Events: Qualitative Findings from a Clinical Event Debriefing Pilot Study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 403.4263
Rita Dadiz, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States; Len Y. Tanaka, University of Hawaii, John A. Burns School of Medicine, Honolulu, HI, United States; Debra L.. Weiner, Boston Children's Hospital/Harvard Medical School, Boston, MA, United States; Daniel Chiou, Cedars-Sinai Medical Center, Los Angeles, CA, United States; Julie Riccio, University of Rochester School of Medicine and Dentistry, Morristown, NJ, United States; Michelle Olech-Smith, American Academy of Pediatrics, Itasca, IL, United States; Ahmed Moussa, Universite de Montreal Faculty of Medicine, Montreal, PQ, Canada; Noorjahan Ali, University of Texas Southwestern Medical School, Dallas, TX, United States; Shiva Zargham, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Natasha Afonso, Texas Children's Hospital, Houston, TX, United States; Doug Dannaway, University of Oklahoma College of Medicine, Edmond, OK, United States; Renuka Mehta, Medical College of Georgia at Augusta University, Augusta, GA, United States; Heather Wolfe, The Children's Hospital of Philadelphia, Wynnewood, PA, United States; Traci Wolbrink, Boston Children's hospital, Boston, MA, United States; Taylor L. Sawyer, University of Washington, Kenmore, WA, United States; Marjorie White, Heersink School of Medicine, UAB, Birmingham, AL, United States; Joseph O. Lopreiato, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Louis Halamek, Stanford University School of Medicine, Palo Alto, CA, United States; Theodora Stavroudis, Cedars-Sinai Guerin Children's and UCLA Geffen School of Medicine, Los Angeles, CA, United States
Rita Dadiz, DO (she/her/hers)
Professor of Pediatrics
Golisano Children's Hospital at The University of Rochester Medical Center
Rochester, New York, United States
Presenting Author(s)
Background: The Neonatal Resuscitation Program® (NRP®) endorses conducting post-resuscitation team debriefings as a constructive review of patient care and team function.
Objective: To qualitatively explore the strengths, weaknesses, and action plans identified from the CEDs of neonatal stabilization events at three academic institutions that implemented a standardized national framework on CED.
Design/Methods: A 17-member American Academy of Pediatrics (AAP) taskforce on clinical event debriefing (CED) developed the “Who, What, When, Where, Why and How in CED” (WHiCED) Program, an iteratively revised standardized CED framework. Three taskforce institutions piloted the standardized use of this framework by conducting CEDs after neonatal resuscitations of newborns who were born at < 29 weeks’ gestation and who received positive pressure ventilation in the delivery room or the neonatal intensive care unit. Strengths, weaknesses, and action plans identified by teams were tracked and entered into a central online data repository as qualitative data. Two taskforce members independently coded data and engaged in thematic analysis.
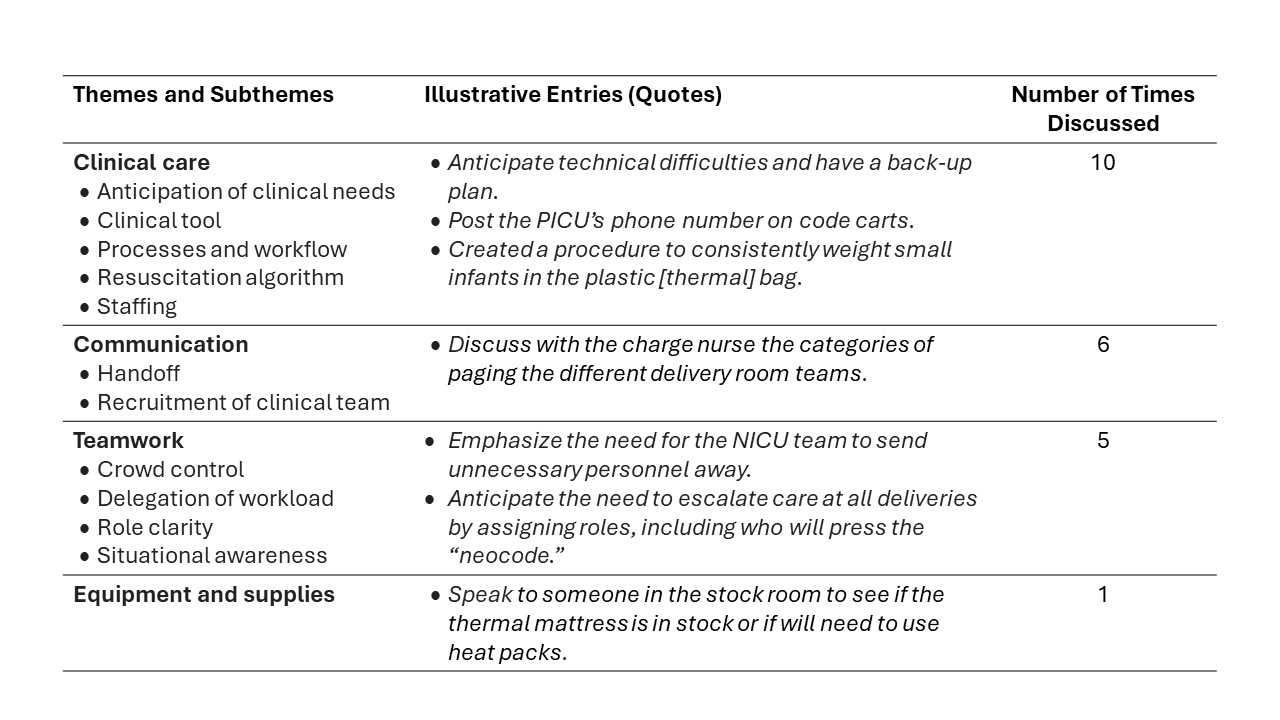
Results: A total of 24 CEDs were conducted at three hospitals with level IV NICUs over a 6-month pilot study period. Behavioral skills were cited as the most common weakness and strength during CEDs (Tables 1-2). Sites provided qualitative comments on discussion points during CEDs, which were categorized into 40 strengths (Table 1), 44 weaknesses (Table 2), and 22 action plans (Table 3). While clinical care was discussed, most discussion points focused on behavioral skills during clinical events, specifically as teamwork and communication practices such as role clarity, situational awareness, handoff communication. Teams discussed the role of continuing professional development, including the use of simulation, as a method to sustain strengths and correct weaknesses identified from CEDs.
Conclusion(s): The majority of strengths and weaknesses discussed by teams during CEDs of neonatal resuscitation events focused on behavioral skills, rather than technical performance. NRP training could benefit from expanding current training modules to address behavioral skills identified as weaknesses during CEDs. Establishing and utilizing a standardized CED database across institutions can assist with identifying best practices, targets for intervention, and quality improvement benchmarks in newborn resuscitation.
Table 1. Themes and Illustrative Entries of Strengths Identified from Clinical Event Debriefings
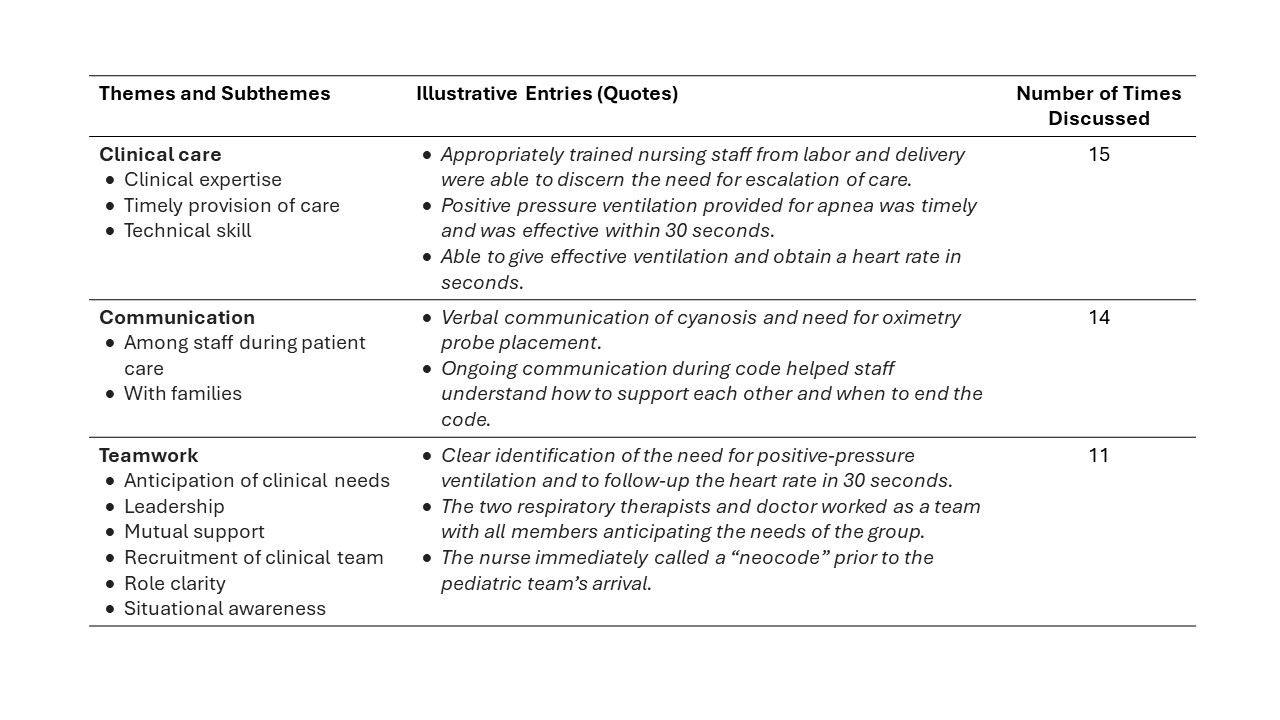
Table 2. Themes and Illustrative Entries of Weaknesses Identified from Clinical Event Debriefings
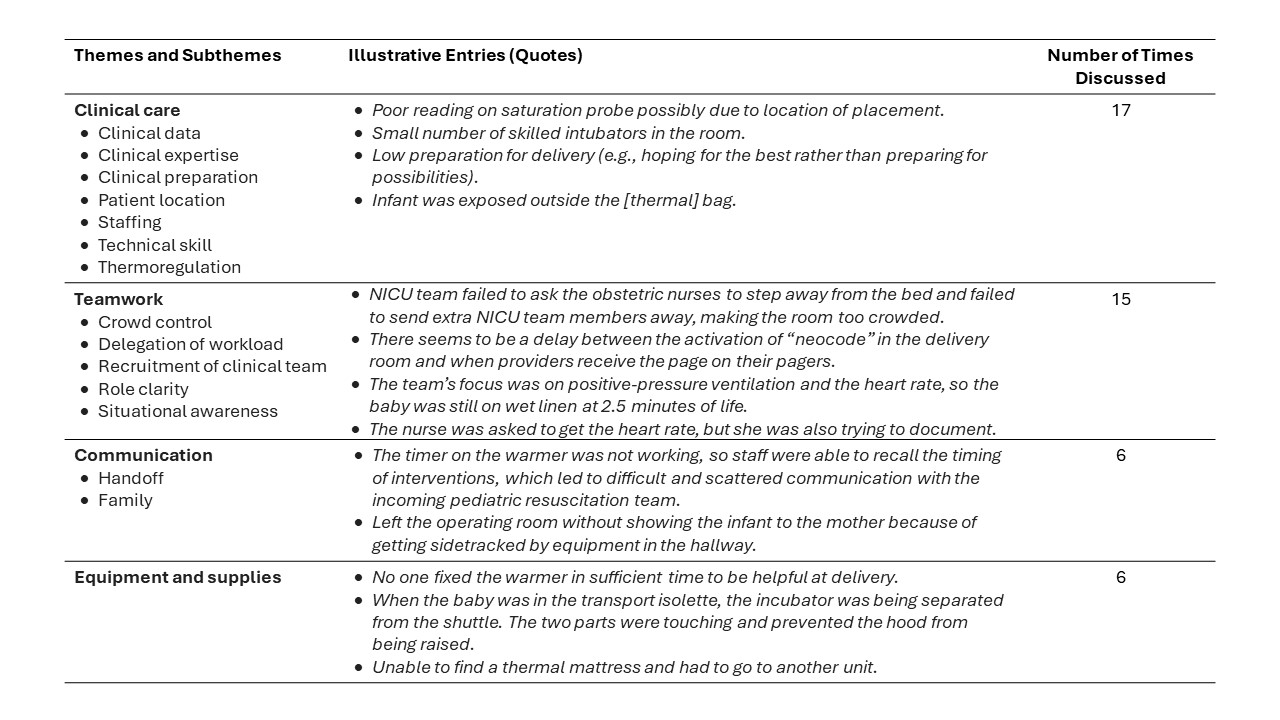
Table 3. Themes and Illustrative Entries of Action Plans Identified from Clinical Event Debriefings